- Be able to identify the parts of the pituitary gland, and describe their embryological origin.
- Name the cell types that produce the various hormones of the anterior pituitary, and know whether they are acidophils or basophils.
- Describe the role of hypothalamic neurosecretion in the function of the posterior pituitary, and in the regulation of the anterior pituitary, and recognize the histological structures involved in these functions.
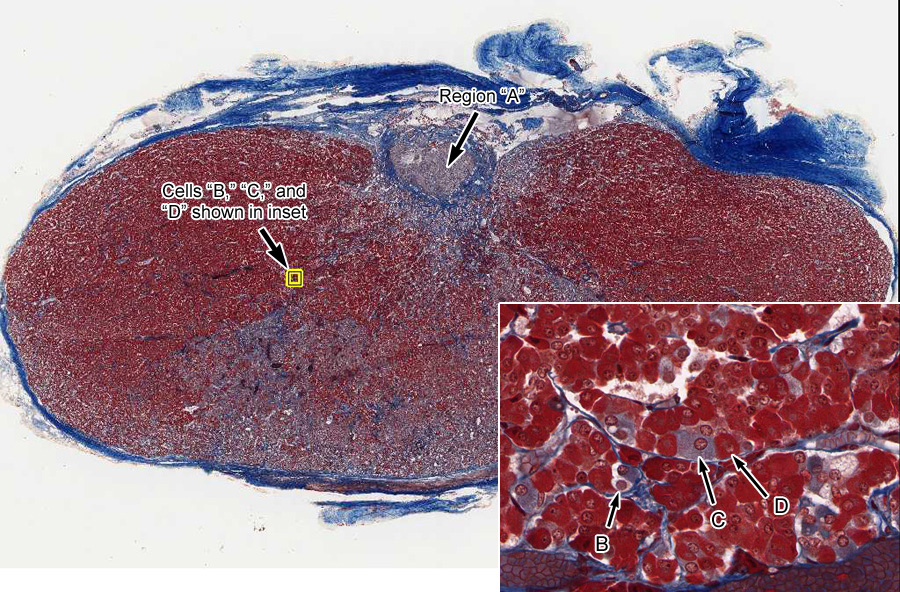
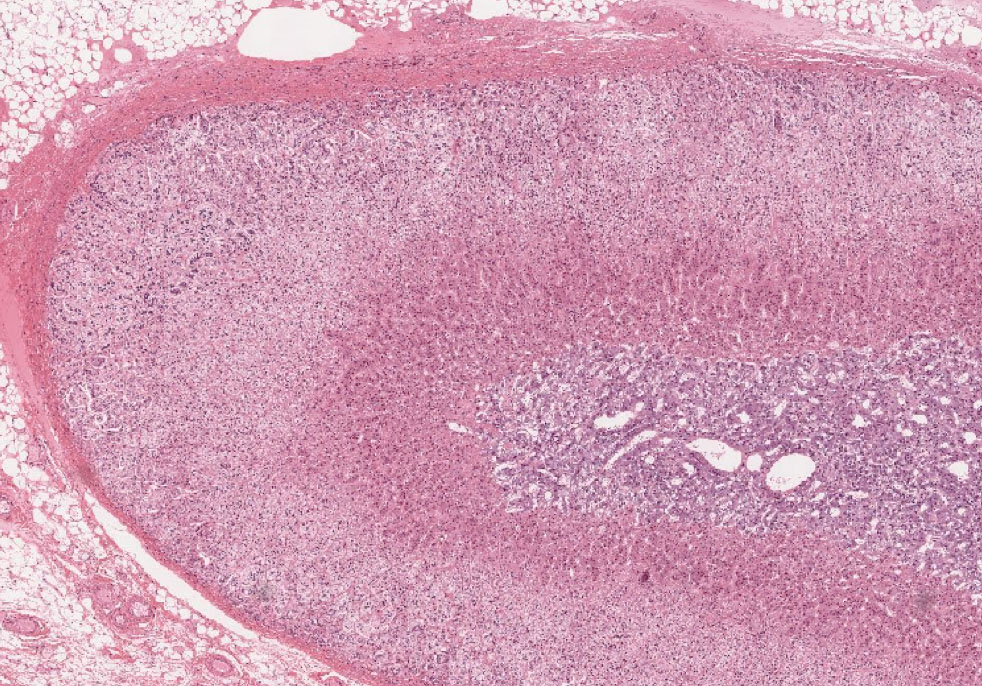
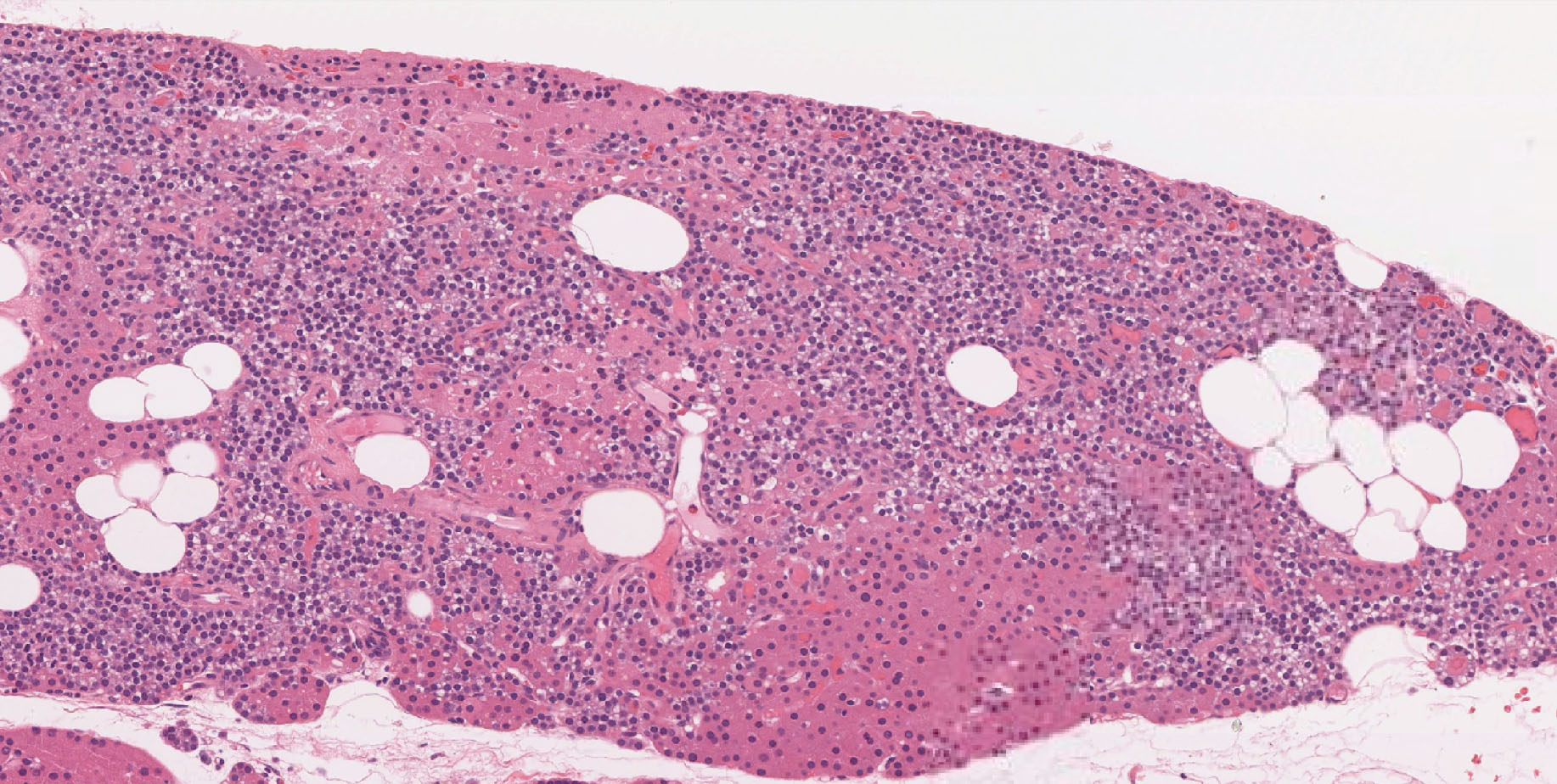
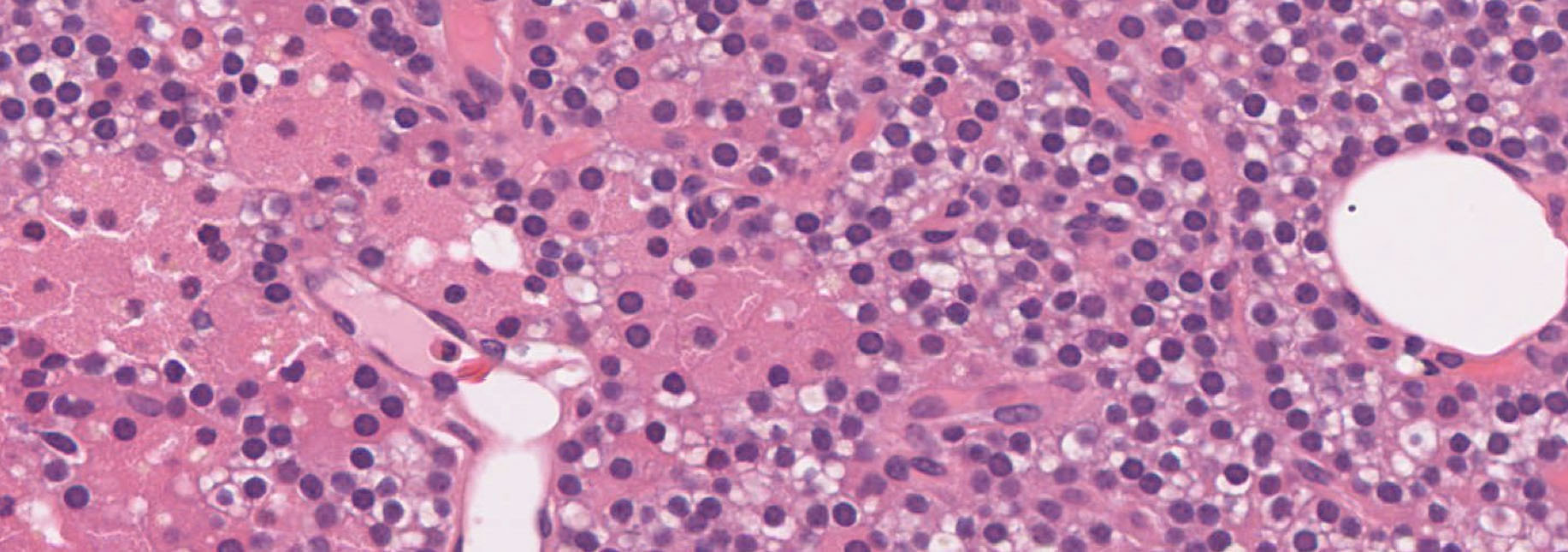
These slides show mostly pars distalis, but also have a small area of neurohypophysis (either pars nervosa or infundibular stalk) on one side (see slide orientation diagrams) and are stained in alternate sets with H&E or with Masson trichrome. The two classes of anterior pituitary cells (acidophils and basophils) are most easily distinguished with Masson trichrome staining, but you should also see how they look with routine H&E staining.
A. Pars distalis (aka anterior pituitary or adenohypophysis)
Slide 226 Pituitary gland Masson cross View Virtual Slide [see orientation]
Slide 226 Pituitary gland H&E cross View Virtual Slide
Slide 226 Pituitary gland H&E sagittal View Virtual Slide [see orientation]
Slide 227 Pituitary gland Masson sagittal View Virtual Slide [see orientation]
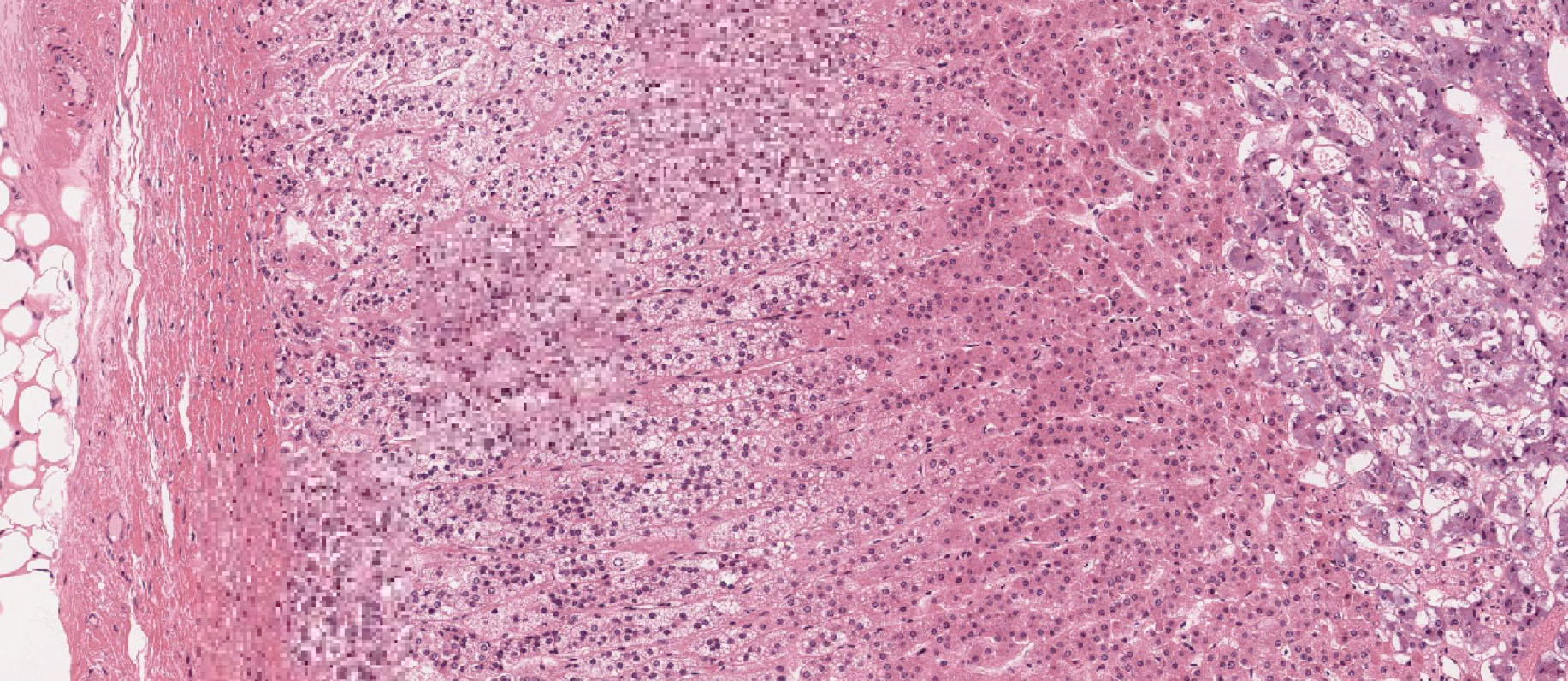
Study the pars distalis (anterior lobe) in the slide stained with Masson trichrome slide 226 pars distalis View Image. The cells are arranged in irregular clusters or cords and are distinguishable by their staining as either acidophils, basophils, or chromophobes. Theacidophils stain red or orange-red, while the basophils stain various shades of blue or blue-gray. Remember that the acidophils include two different cell types, somatotropes (growth hormone) and mammotropes (prolactin), while the basophils include gonadotropes (FSH and LH), thyrotropes (TSH) and corticotropes (ACTH). ACTH is actually a cleavage product of pro-opiomelanocortin (POMC), which is made by corticotropes and processed primarily into ACTH in these cells. To a lesser extent, corticotropes also produce other signaling factors derived from POMC such as lipotropins (involved in lipid metabolism), endorphins (endogenous opioids that reduce pain perception), and melanocyte stimulating hormone (MSH). Occasional cells in the anterior pituitary show no distinctive staining and are called “chromophobes”. You will only be required to distinguish acidophils from basophils. Your best strategy is first to identify acidophils, which are more distinctively stained, and then the remaining cells are almost entirely basophils. The cells are not uniformly distributed throughout the pars distalis, but instead there are areas where acidophils predominate, other areas where basophils are more numerous, while still other regions may show a more even mixture of acidophils and basophils. Note the abundant sinusoidal capillaries (often filled with red blood cells) slide 226 sinusoidal capillaries View Image that lie between the cell cords or clusters. You can appreciate how readily the hormones secreted from the cells can reach the blood. Since collagen stains bright blue with the Masson trichrome method, you can see the delicate connective tissue partitions between cords and around blood vessels. In the routine H&E-stained sections, you can also identify acidophils and basophils, although the difference is not as obvious as it is with Masson trichrome staining. Here again, you should first identify acidophils, which stain various shades of reddish pink, and then the remaining cells are almost entirely basophils, which vary generally from bluish/grayish-pink to blue.
B. Pars nervosa (aka posterior pituitary or neurohypophysis)
Slide 227 Pituitary gland monkey Masson cross View Virtual Slide [see orientation]
Slide 227 Pituitary gland monkey H&E cross View Virtual Slide [see orientation]
Slide 227 Pituitary gland Masson sagittal View Virtual Slide
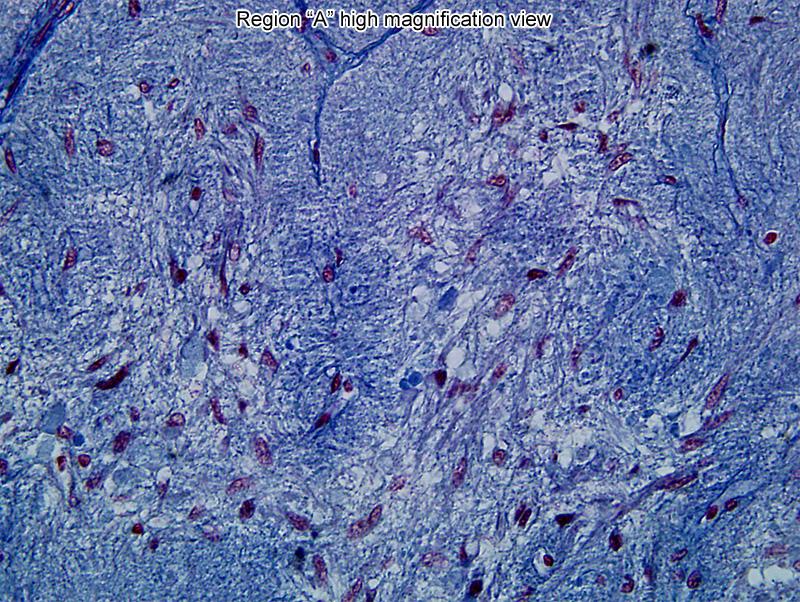
Although the pars nervosa can be found on the human pituitary slides in our collection, the monkey pituitary specimens (H&E and trichrome-stained) contain a significant portion of the pars nervosa (posterior lobe) and are probably better for studying this tissue. The pars nervosa looks like brain tissue, which it is. It is an extension of the brain, composed primarily of nerve fibers (axons) which originate from nerve cell bodies in the hypothalamus and pass to the pars nervosa by way of the hypothalamo-hypophyseal tract and the infundibular stalk. These nerve fibers carry oxytocin and antidiuretic hormone (ADH, vasopressin) to nerve endings, from which they are released into nearby capillaries upon neural stimulation from the hypothalamus. There is not much to see in the posterior lobe in these histological sections. Since there are no neuron cell bodies in this structure, most of the prominent nuclei belong to pituicytes , which are the characteristic glial cells of the pars nervosa. You will also see the nuclei of blood vessel endothelial cells , and fibroblasts which are in the connective tissue around these vessels.
C. Pars intermedia
Slide 227 Pituitary gland monkey Masson cross View Virtual Slide
Slide 227 Pituitary gland monkey H&E cross View Virtual Slide
Slide 226 Pituitary gland H&E sagittal View Virtual Slide
Slide 227 Pituitary gland Masson sagittal View Virtual Slide
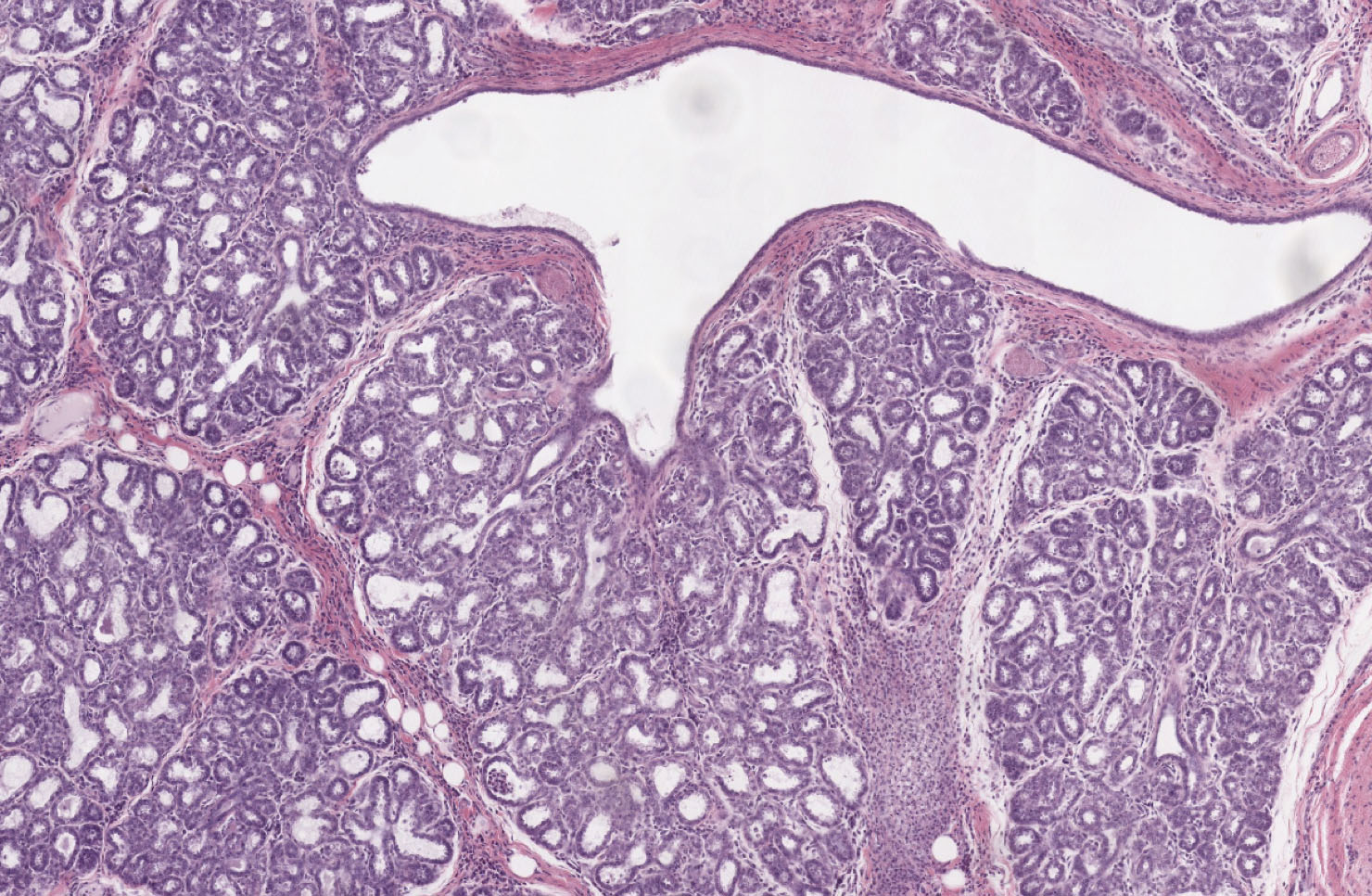
The pars intermedia is very poorly developed in the human pituitary, but is prominent in the pituitaries of most other mammals. For example, in the monkey pituitary, you will see the pars intermedia as a prominent layer several cells thick, lying between the pars distalis and pars nervosa. In some places you may also see a long cleft between the pars distalis and the pars intermedia, which is a substantial remnant of the lumen of the embryonic Rathke’s pouch, an ectodermal outpocketing of the oral cavity which gave rise to both the pars distalis and the pars intermedia. Cells of the pars intermedia also produce POMC (pro-opiomelanocortin), which in these cells is processed primarily into endorphins and MSH (melanocyte stimulating hormone). In contrast to its substantial presence in other mammals, the pars intermedia of the human pituitary is usually represented merely by a thin layer of basophilic cells that can be seen in both the human trichrome and H&E-stained human sections lying against the pars nervosa, and is probably of little functional importance. Between the pars intermedia and pars distalis are occasional fluid-filled cysts (again visible in both trichrome slide 227 View Image and H&E-stained slide 226 View Image sections), which are the only vestiges of the lumen of Rathke’s pouch. Although most of the human axial sections in your sets do not show the human pars intermedia very well, the sagittal sections in some of the sets show some indication of it.
D. Infundibular stalk and hypophyseal portal vessels
Slide 229B Infundibular stalk, and hypophyseal portal vessels H&E View Virtual Slide [see orientation]
Slide 229 Infundibular stalk, hypophyseal portal vessels H&E View Virtual Slide
This slide shows the hypophyseal portal blood vessels slide 229 View Image that carry releasing hormones from the hypothalamus to regulate the release of hormones from the pars distalis of the pituitary. Look for these prominent blood vessels in portions of the pars distalis that extend up around the infundibular stalk. In many of these slides the sinusoidal capillaries slide 229 View Image lying between cords of pituitary cells throughout the anterior pituitary are shown particularly well. Scan over the slide, reviewing other features you saw in slides 226 and 227 (e.g. acidophils vs. basophils; neurohypophysis vs. adenohypophysis).
232 Adenohypophysis - Survey of cell types Adenohypophysis – Anterior Pituitary View Virtual EM Slide
Here you see pituitary cells of various size clustered between capillaries. The main cell types are somatotropes (GH), mammotropes (prolactin), gonadotropes (FSH and LH), thyrotropes (TSH) and corticotropes (ACTH). You will not be required to identify these cell types in electron micrographs, but should note that the cells differ in size, shape and in the number, size and distribution of their secretory granules (small black structures in the cytoplasm). When the content of a secretory granule is released from the cells, the hormones diffuse to nearby capillaries. The endothelium of these capillaries is very thin and, as with most endocrine organs, contains fenestrations (not seen clearly in this micrograph).
233 Adenohypophysis - Detail of some cell types Adenohypophysis – Anterior Pituitary View Virtual EM Slide
This electron micrograph shows two of the pituitary cell types in more detail. Two gonadotropes occupy most of the lower half of the figure. Two somatotropes take most of the middle and upper portion of the image. Hormones are synthesized on the rough endoplasmic reticulum (RER) of the two cell types. The hormone subsequently passes through the Golgi complex and is then directed and collected into secretory granules. Since FSH and LH are glycoproteins, terminal sugars are added to the oligosaccharide chains as the hormone passes through the Golgi stack. When a cell is stimulated by appropriate releasing hormone from the hypothalamus, the content of the granules is released from the cell by exocytosis.
234 Adenohypophysis – Anterior Pituitary View Virtual EM Slide.
Note the fenestrated capillaries and that the secretory granule content is discharged by exocytosis (through the fusion of the secretory granule membrane with the cell membrane).
235 Neurohypophysis – Posterior Pituitary View Virtual EM Slide.
Note the Herring bodies at axonal endpoints close to capillaries, microglial cell, and pituicyte.
Click on a question to reveal the answer.
What would be the most pronounced histological difference between the pituitaries of castrated and non-castrated males (assuming no hormone replacement)?
First consider the products of the cells in the anterior pituitary. Acidophils include somatotropes (produce growth hormone) and mammotropes (produce prolactin). Basophils are either thyrotropes (produce TSH), gonadotropes (produce LH and FSH) or corticotropes (produce ACTH). Basophilic cells are all regulated by feedback inhibition, where the products of the target organs they stimulate can act directly on the anterior pituitary to downregulate the production of the initial hormone (LH, FSH, TSH, and ACTH). In castration, the cells in the testis that are normally stimulated by LH and FSH are gone and can’t produce hormones to downregulate their production. Instead, the absence of negative feedback causes an increase in LH and FSH produced by the basophilic gonadotropes of the anterior pituitary. These cells subsequently hypertrophy in a vain attempt to induce some type of response in the testis (which are no longer there). Histologically, this is seen as hypertrophy and increased numbers of basophils in the anterior pituitary. Now see if you can figure out what would happen to the pituitary if other glands were removed (for example the thyroid).
What would happen to the various endocrine glands in the absence of hormone production by the anterior pituitary (for example hypophysectomy)?
The anterior pituitary produces hormones that directly stimulate the mammary glands, the adrenal glands, the thyroid, and the ovaries or testis. Removal of GH, PRL, ACTH, TSH, FSH and LH from the system would have varying effects. Loss of ACTH would lead to the collapse of the adrenal cortex and a nearly complete loss of production of glucocorticoids and some weak androgens. The lack of prolactin would lead to decreased milk production in mammary glands. Without TSH, the follicular cells of the thyroid would shrink, leading to hypothyroidism. In the gonads, FSH and LH are essential in producing androgens and estrogens necessary for reproduction. The loss of these two hormones would prevent the maturation of eggs or sperm in the gonads as well as hinder the development of secondary sex characteristics.
- Explain how structures seen in the thyroid gland, at both the light and electron microscope levels, are involved in the production of thyroglobulin, its storage, and its subsequent breakdown to yield thyroid hormones.
- Recognize the parathyroid gland in histological section, and within the gland identify the chief cells (source of parathyroid hormone) and oxyphil cells.
Slide 217 Thyroid gland, parathyroid H&E View Virtual Slide
Slide 218-norm Thyroid gland rat Masson View Virtual Slide
Slide 218-hypo Thyroid gland rat hypoactive Masson View Virtual Slide
Slide 218-1 Thyroid gland rat hyperactive Masson View Virtual Slide
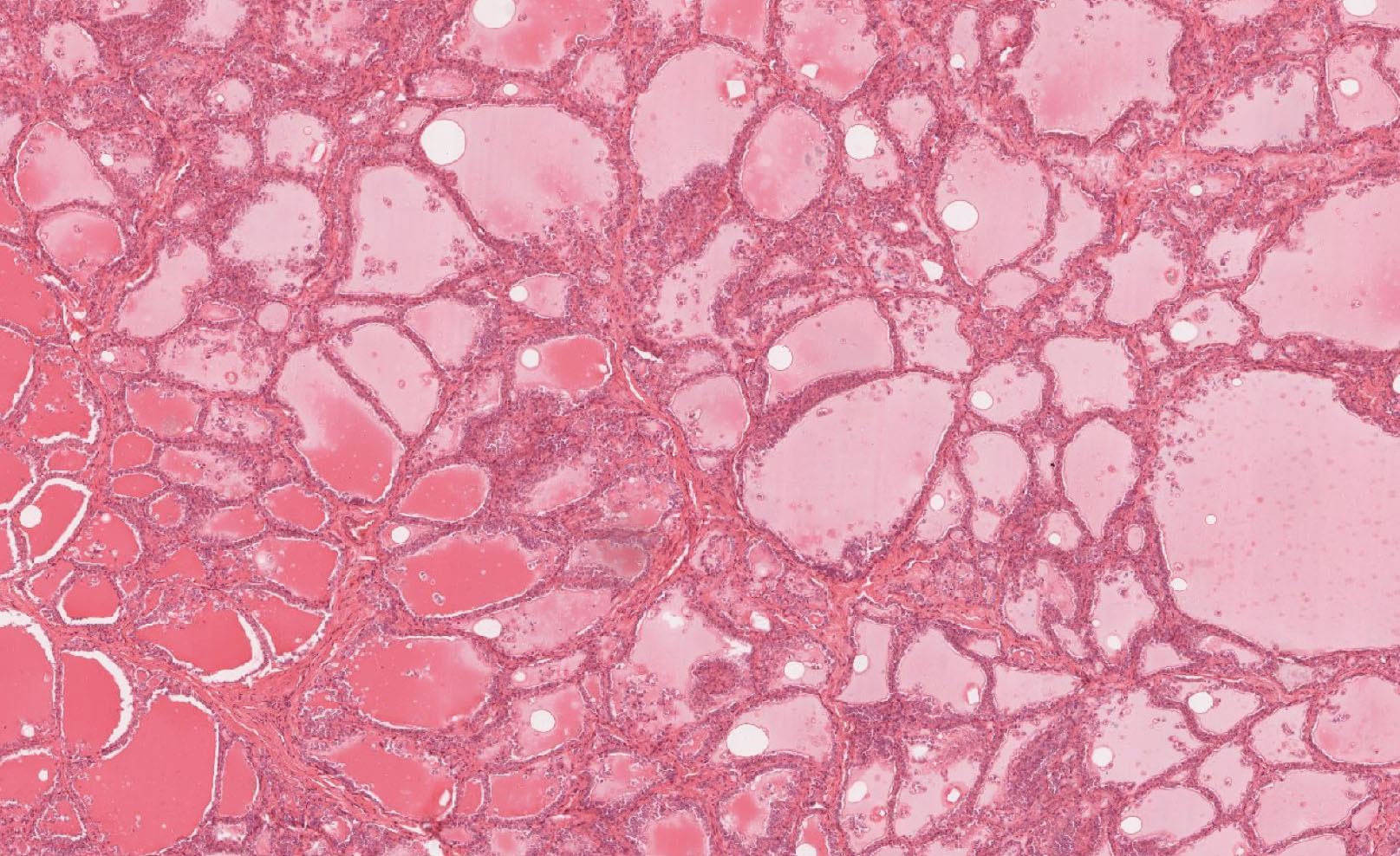
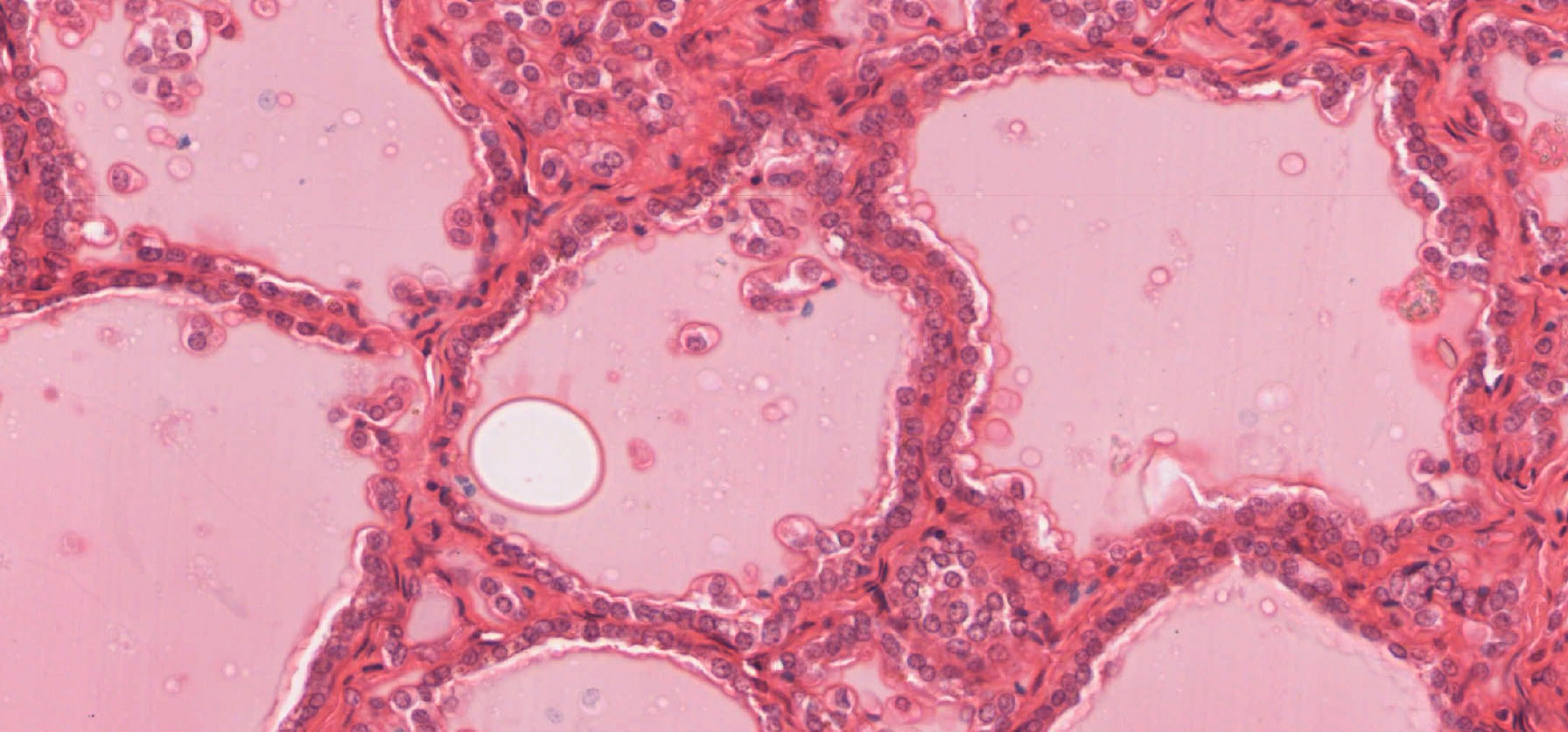
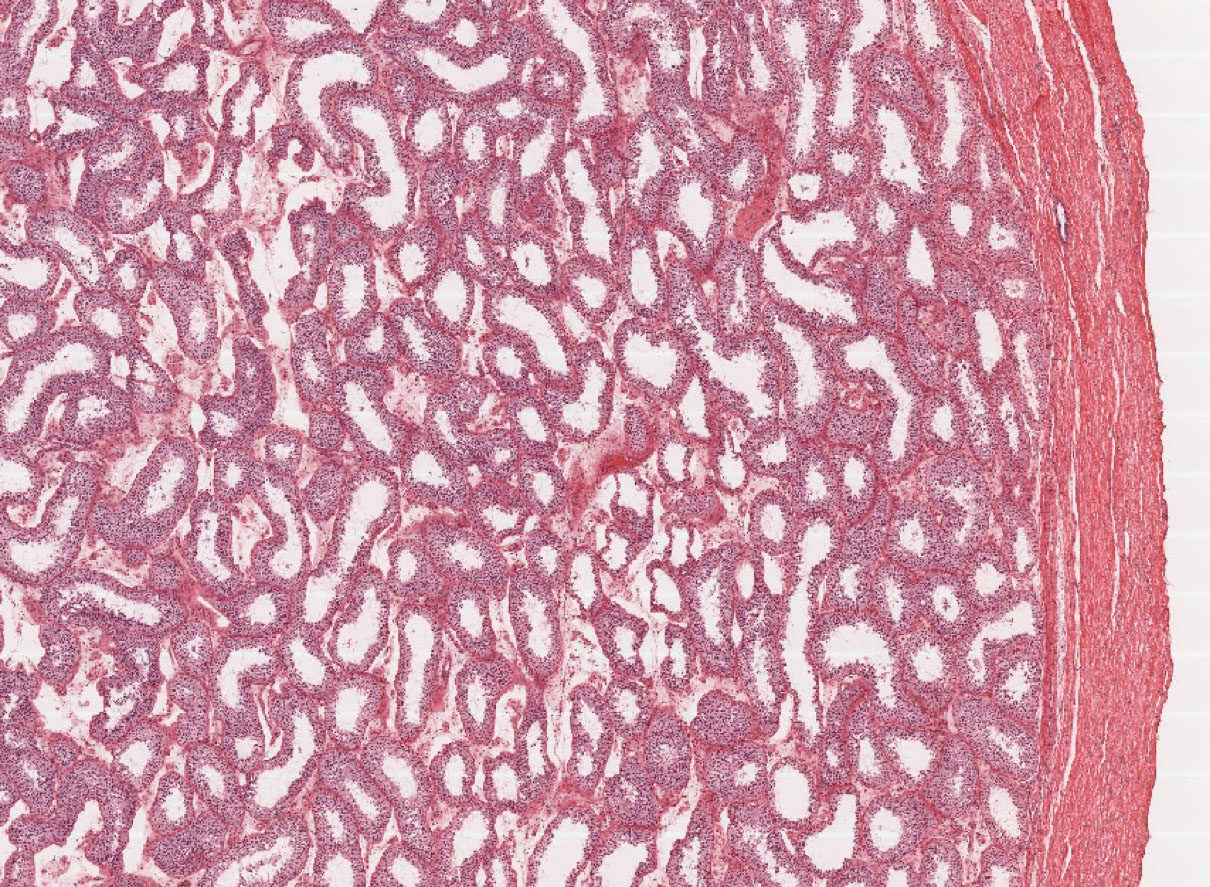
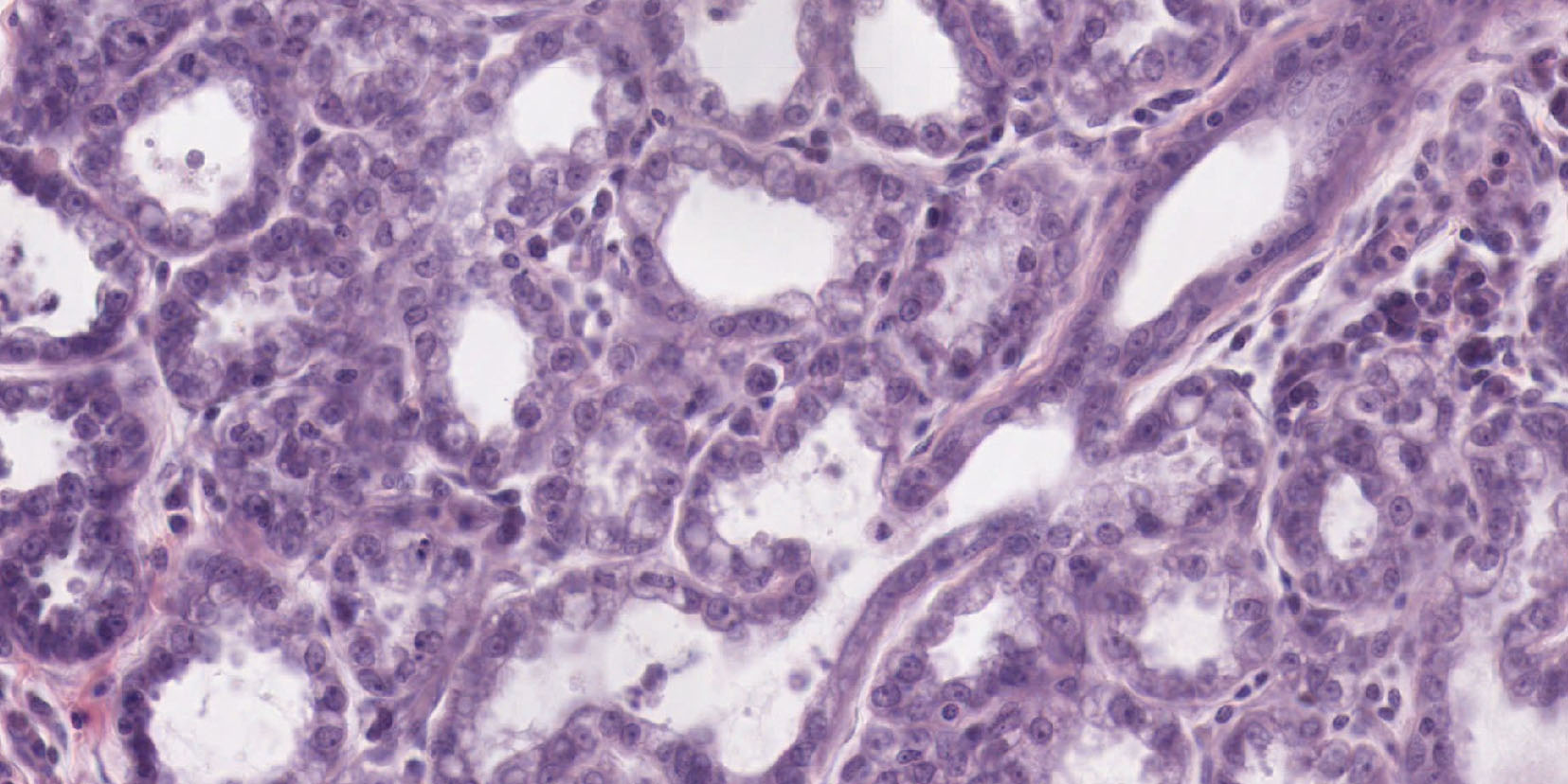
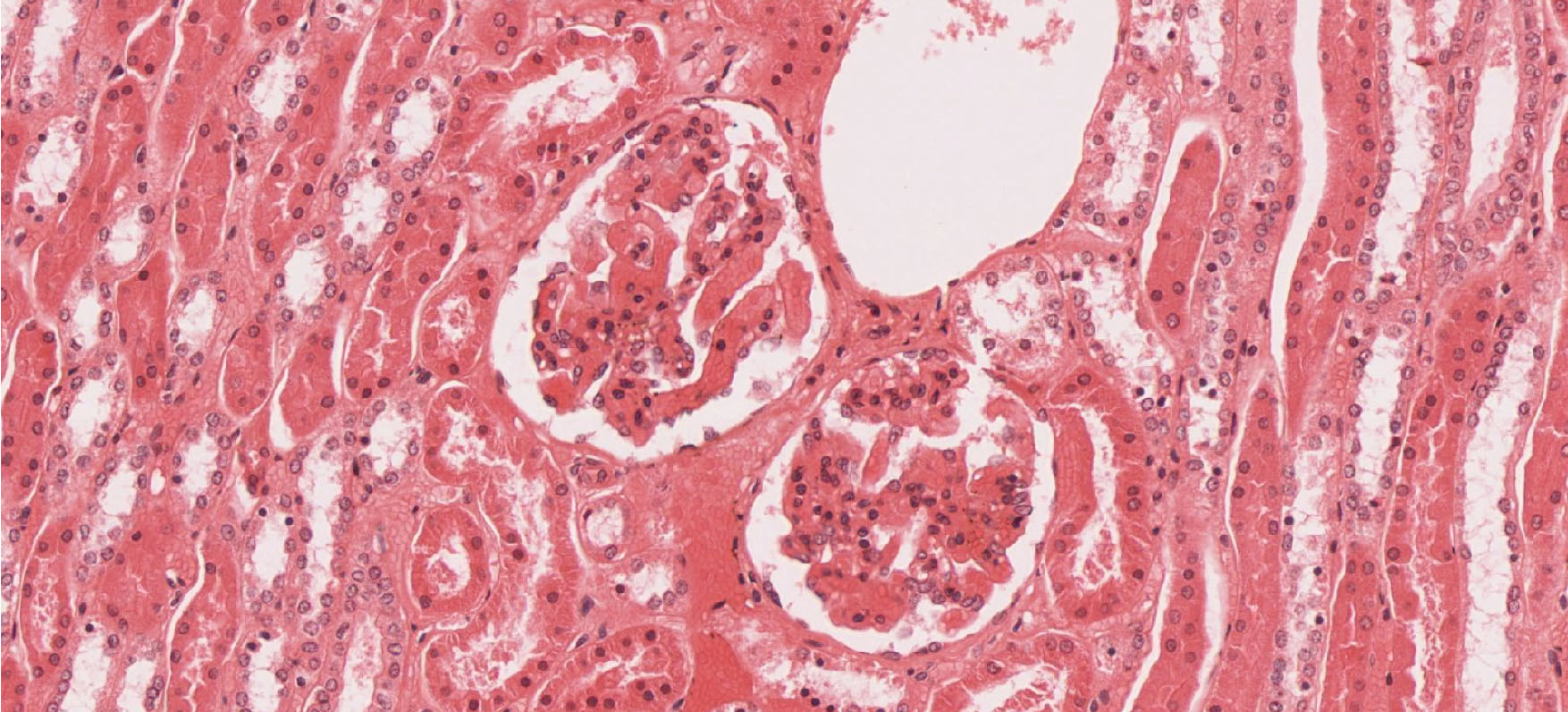
Examine slide 217 at low magnification, then at higher magnifications. Note that the thyroid gland is made up of functional units calledfollicles, which in three dimensions are approximately spherical, their walls being composed of a simple cuboidal epithelium, surrounding a lumen that contains colloid. Note that the follicles vary in size and that the height of the follicular epithelial cells may also vary. The colloid is composed primarily of thyroglobulin, a glycoprotein synthesized by the follicular epithelium. Under stimulation from pituitary TSH, the thyroid cells break down the thyroglobulin to release thyroid hormones (T3 and T4), which pass into nearby capillaries. Occasional parafollicular cells (C-cells), source of the hormone calcitonin, are also present between the follicles and in the follicular epithelium slide 217 View Image. However, they are difficult to distinguish in routine histological slides of human thyroid, and you are NOT expected to recognize them based on light microscopy alone (but you should know that they are the source of calcitonin which is packaged into secretory granules that makes these cells readily identifiable by electron microscopy). There are three versions of slide 218 that show a rodent thyroid at three different levels of functional activity: (1) normal slide 218-1 View Image, (2) hypoactivity due to hypophysectomy slide 218-hypo View Image, and (3) hyperactivity slide 218-hyper View Image due to treatment with the drug thiouracil. Compare the tissue shown in each slide --the variation is not overwhelming since the experiments were performed conservatively, but you should be able to see some differences in epithelial cell height and in the size of the follicular lumens. After hypophysectomy there is no stimulation by TSH, so the follicular epithelial cells become reduced in height and the colloid in the lumen is abundant, since it is not being resorbed to make thyroid hormones (in these hypoactive slides, slide 218-hypo View Image , C-cells are more obvious as these cells are fully functional and not dependent on TSH). In contrast, in the hyperactive follicles of thiouracil-treated animals the epithelium is columnar, and the follicular lumen is much reduced in size. The reason for this hyperactivity is that thiouracil blocks the oxidation of iodide, with the result that functional thyroid hormones can no longer be produced. The lack of thyroid hormones in the blood stream leads to stimulation of the pituitary to produce large quantities of TSH, causing the thyroid follicular cells to hypertrophy and resorb colloid very actively from the lumen, reducing its size. The frantic effort of these cells is futile, however, since the oxidized iodine necessary to make functional thyroid hormones is unavailable.
Slide 217 Thyroid gland, parathyroid H&E View Virtual Slide [see orientation]
Slide 220 Parathyroid H&E View Virtual Slide
Slide 221 Parathyroid H&E View Virtual Slide
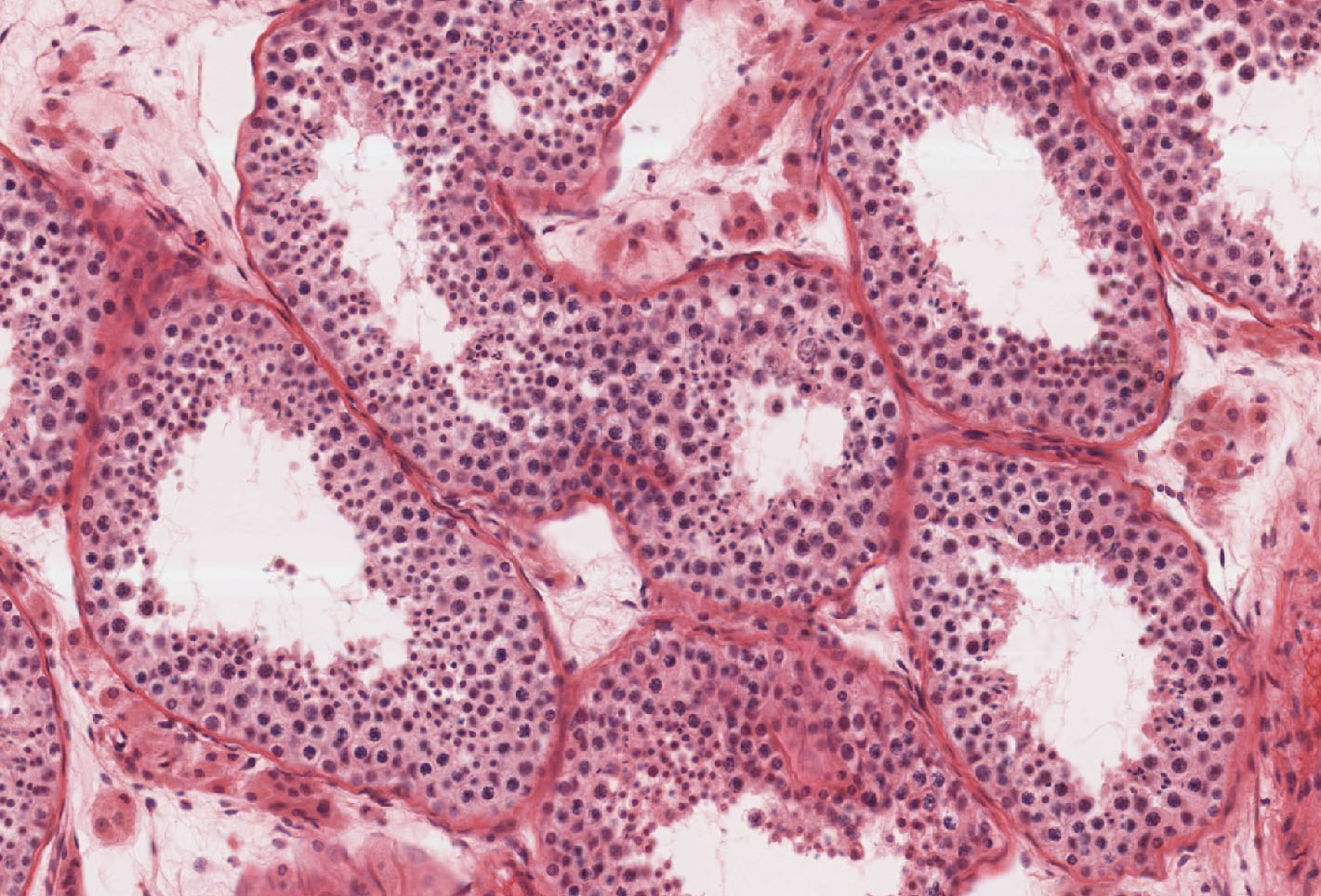
Sections of parathyroid gland can be seen on slides 217, 220, and 221. In slide 217, parathyroid tissue will be found on one side of the much larger mass of thyroid tissue. To find the parathyroid tissue on slides 217, scan around the periphery of the thyroid tissue at low magnification. (Note: slide 217 in a few of the glass slide sets lacks parathyroid.)
The parenchyma of the gland slide 217 View Image is made up of two identifiable cell types: the predominant chief (or principal) cells (source of parathyroid hormone) and occasional oxyphil cells. Observe the arrangement of chief cells in the parathyroid as seen on slides 217, 220, and 221. The chief cells are arranged as interconnecting cords or clusters, with blood vessels and connective tissue forming the partitions between the cell cords. The capillaries in slide 221 may be more easily seen because erythrocytes have been retained within the lumens. The individual chief cells, seen well in slide 220, have relatively little cytoplasm, which may be almost unstained or lightly basophilic. The lightly stained cells are thought to be quiescent while the more basophilic cells are believed to be more actively involved in the synthesis and secretion of parathyroid hormone.
In either slide 217, 220, or 221 try to find oxyphil cells. Oxyphil cells are much less numerous than chief cells, and can be differentiated from them by the following criteria: (1) larger than chief cells, with more extensive, eosinophilic cytoplasm, (2) nuclei smaller and darker staining, (3) usually occur in isolated groups. Not every specimen in the glass slide sets contain readily identifiable oxyphil cells, but they can be found on each of the virtual slides: slide 217 View Image, slide 220 View Image, and slide 221 View Image.
241 Thyroid Gland View Virtual EM Slide
The gland is made up of follicles, with epithelial cells forming their walls and containing a lumen full of colloid. The follicles vary in size. Parafollicular cells, which secrete calcitonin, are present in between follicles and can be distinguished at the EM level. However, it is difficult to recognize them at the LM level. Also note the numerous capillaries closely apposed to the follicles, which is a characteristic of endocrine tissues.
242 Thyroid Gland - Thyroid Follicular Cell View Virtual EM Slide
Remember that the follicular cells secrete thyroglobulin into the colloid and subsequently resorb it and break it down to produce thyroid hormones. In this electron micrograph, try to identify the various organelles and cellular structures involved in these functions.
243 Thyroid Gland - Parafollicular Cell View Virtual EM Slide
Note that the cell is surrounded by follicular cells and contains numerous small and electron-dense secretory granules.
246 Parathyroid Gland View Virtual EM Slide The gland consists of cords of chief cells with occasional islets of oxyphil cells, which are filled by abundant mitochondria.
Click on a question to reveal the answer.
What would be the appearance of the thyroid of a person with Graves disease?
As you will learn in the immune system sequence, Graves disease is a type II immune response that targets thyroid stimulating hormone (TSH) receptors on the thyroid. Even though the excessive T3 and T4 in the blood stream downregulate the production of TSH, antibodies continue to stimulate the receptors causing an increase in T3 and T4 production. Graves disease is essentially a form of hyperthyroidism and, as such, would show hypertrophic epithelial cells and profoundly scalloped colloid within the follicles.
What hormone is secreted by the parafollicular cells of the thyroid and what hormone produces the opposite physiological effect?
Parafollicular cells are involved in the production of calcitonin, which lowers blood calcium levels by preventing bone resorption. The hormone with the opposite effect as this is parathyroid hormone (PTH, made by chief cells in the parathyroid), whose production is triggered by low levels of calcium in the blood and which acts to raise calcium levels by stimulating osteoclasts and the resorption of bone.
- Recognize the zones of the adrenal cortex that produce aldosterone and cortisol, and explain how the blood supply is arranged for efficient uptake of the hormones.
- Recognize the adrenal medulla in histological section, and explain the functional similarity of its cells to those of the sympathetic nervous system.
Slide 230 (adrenal gland, human, H&E) View Virtual Slide [see orientation]
Slide 231 (adrenal gland, monkey, H&E) View Virtual Slide [see orientation]
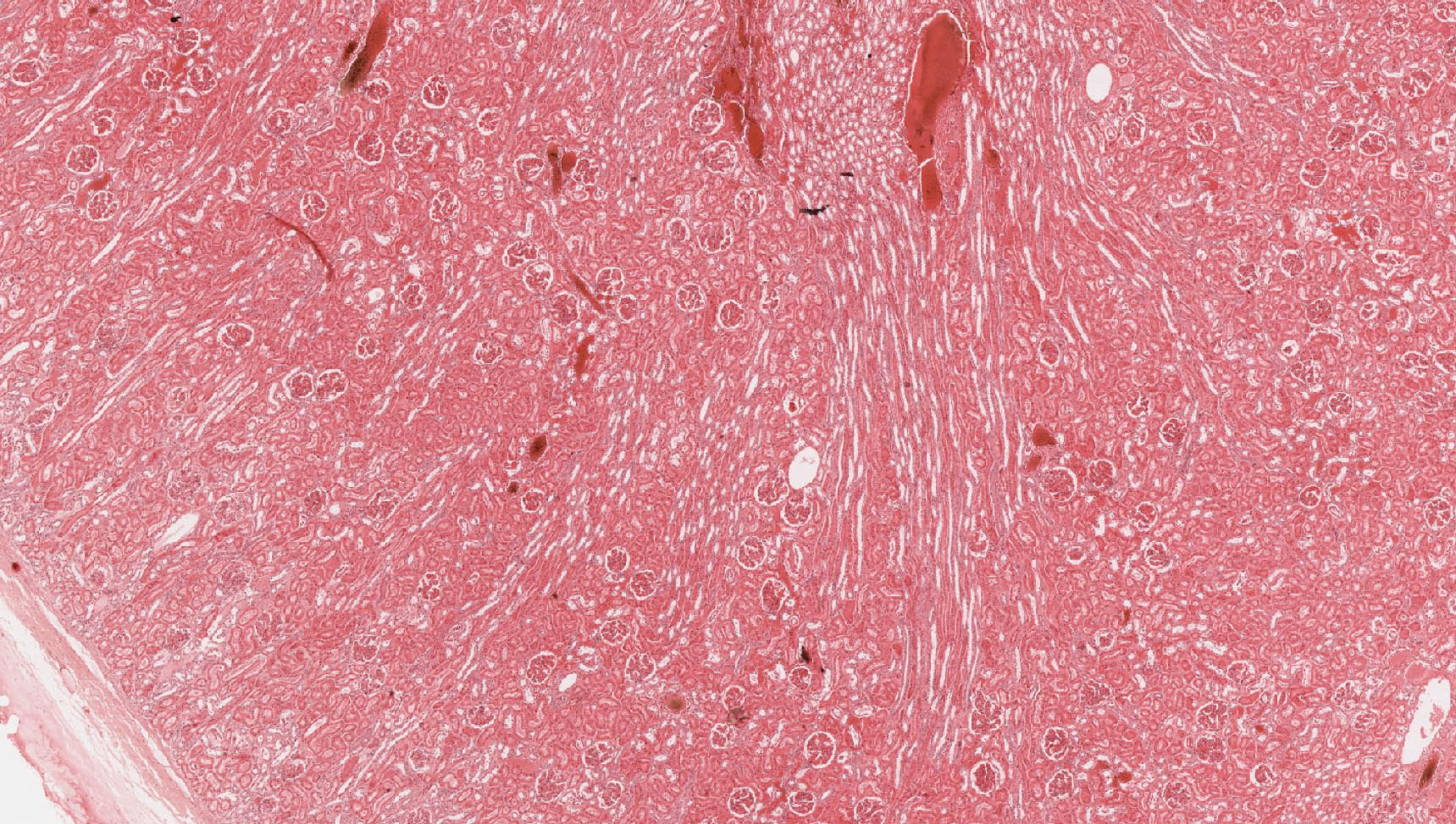
At low magnification on the human adrenal gland (slide 230), note that the gland is enclosed by a connective tissue capsule and has two principal regions - a cortex and a medulla. The cortex View Image occupies the greatest area on your slide. In many regions of slide 230 you will see only cortex, because some parts of the human adrenal lack medulla. The cortex is made up of three regions or zones: the zona glomerulosa, the zona fasciculata and the zona reticularis. The zona fasciculata View Image is probably the easiest layer to spot as it is a broad zone of cells arranged in straight cords, one or two cells thick, which run at right angles to the surface of the gland. The cells of the fasciculata are lightly stained and have a frothy appearance, due to the extraction of lipid droplets from the cell cytoplasm during tissue processing. Interior to the fasciculata is the zona reticularis View Image, which stains more deeply than the other two regions of the cortex. The cells of the zona reticularis are arranged as anastomosing (reticular or net-like) cords. The zona glomerulosa View Image is found outermost in the cortex and consists of cells arranged in rounded or arched clusters although in the human adrenal gland, the zona glomerulosa may not be present around the entire periphery of the cortex. In other species, however, this zone exists as a complete layer around the entire periphery of the cortex as shown in slide 231, which of the monkey adrenal gland. Continuing inward on slide 231, you should be able to recognize the zona fasciculata View Image, zona reticularis View Image, and, finally, medulla View Image. Notice that throughout the cortex of both the human and monkey adrenal glands are numerous capillaries, with somewhat expanded lumens.
Return to the medulla of slide 230 (human adrenal section) View Image. The medullary cells, source of norepinephrine (noradrenalin) and epinephrine (adrenalin), are often more basophilic than the cells of the cortex. The cells of the medulla are considered to be modified postganglionic sympathetic neurons (derived from neural crest cells). These secretory cells are also called chromaffin cells, because their secretory granules (containing norepinephrine or epinephrine) stain brown with potassium dichromate. Note the branches of the central (or medullary) vein View Image in the medulla, and review the blood circulation of the adrenal.
250 Adrenal Cortex View Virtual EM Slide
Note the connective tissue capsule and the zona glomerulosa beneath the capsule. The boundary between the zona glomerulosa and zona fasciculata is not distinct even at the E.M. level. Notice the numerous large capillaries. Clear circles in the cytoplasm are extracted lipid droplets.
254 Adrenal Cortex - Details of a Zona Reticularis Cell View Virtual EM Slide
Note the ultrastructure of these steroid-hormone secreting cells. What is responsible for giving these cells their characteristic light colored, bubbly cytoplasm? (EN7) These cells contain numerous lipid droplets. Notice also that the cells have numerous mitochondria with tubular cristae. Mitochondria with this structure are often found in steroid synthesizing cells. What other organelle, which is not seen well in this micrograph, is also abundant in cells that synthesize steroids? (EN8) Cells in the adrenal cortex are associated with capillaries, which have the fenestrated endothelium that is characteristic of capillaries in endocrine tissues.
255 Adrenal Medulla View Virtual EM Slide
Notice that the cells of the adrenal medulla have smaller mitochondria and also contain numerous distinct secretory granules. Two types of cells are found, one secreting epinephrine (adrenalin), the other secreting norepinephrine (noradrenalin), which you will not be asked to discriminate. Locate nerve endings in contact with the medullary cells.
Click on a question to reveal the answer.
What is the difference between the origin of cells of the cortex and the origin of medullary cells in the adrenal gland?
Cells of the adrenal cortex arise from intermediate mesoderm whereas those of the medulla come from neural crest.
In the medulla, how can you tell which cells secrete epinephrine and which secrete norepinephrine?
You can't at the LM level. Histologically they look the same. However, they can be distinguished at the EM level by a difference in the appearance of their secretory granules. However, you will not be required to distinguish them.
What is responsible for giving the cells of the zona fasciculata their characteristic light colored, bubbly cytoplasm?
The foamy appearance of cells of the zona fasciculata comes from the extracted lipid droplets in the cytoplasm.
What other organelle, which is not seen well in this micrograph, is also abundant in cells that synthesize steroids?
Smooth endoplasmic reticulum is abundant in steroid-synthesizing cells.
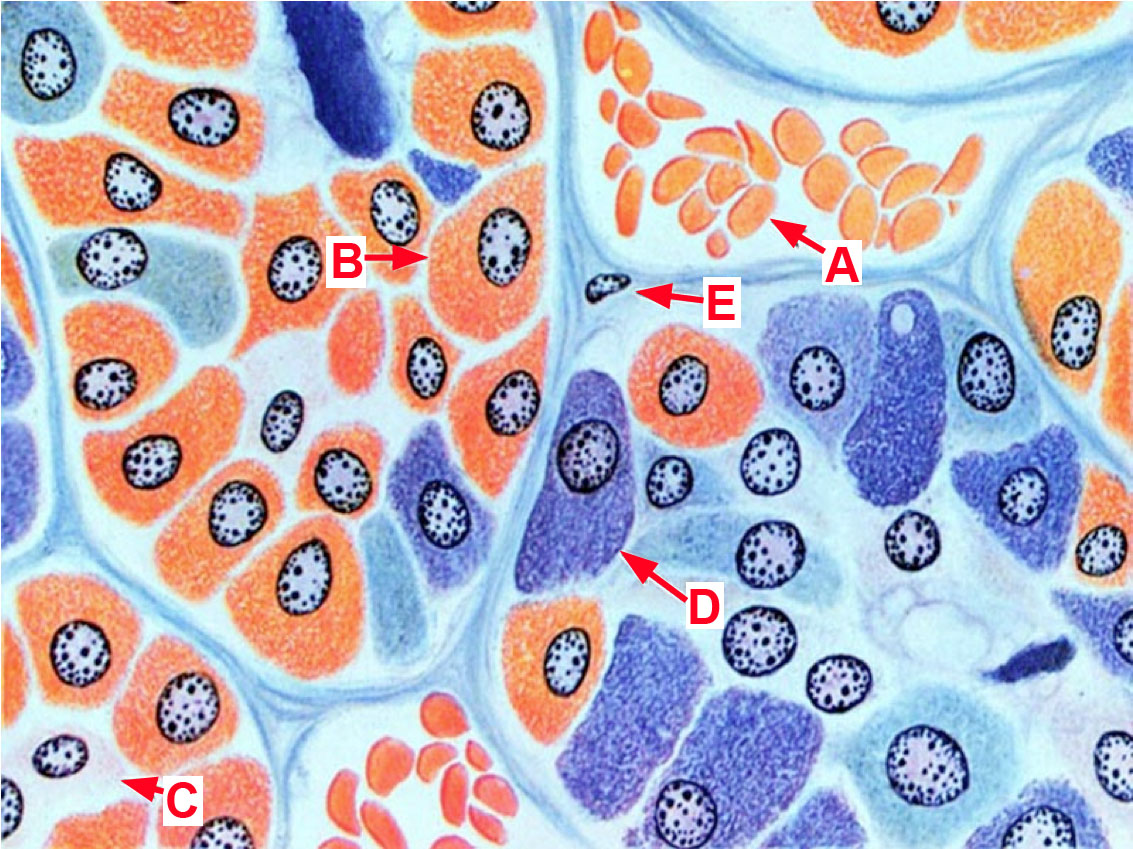
Questions 1 through 6 refer to this trichrome-stained section of the hypophysis.
Match each of the target organs below with the appropriately labeled cell or region of the hypophysis. Each labeled cell or region may be used once, more than once, or not at all. For some target organs, there may be MORE THAN ONE correct answer, in which case you should choose all answers that apply.
1. Match target organ 1
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answer 3., cell type C - The target organ is the thyroid gland, which is regulated by anterior pituitary THYROTROPHS, which are BASOPHILS.
2. Match target organ 2:
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answer 3., cell type C - The target organ is the adrenal gland. Cells of the adrenal cortex (specificially cells of the zona reticularis and fasciculata) are regulated by CORTICOTROPHS, which are BASOPHILS.
3. Match target organ 3
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answer 3., cell type C - The target organ is the testis, which is regulated by GONADOTROPES, which are BASOPHILS.
4. Match target organ 4
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answer is 5, NONE of the above, The target organ is the parathyroid gland, which is not directly regulated by cells of the anterior or posterior pituitary.
5. Match target organ 5
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answers 1. and 4., region A and cell type D. The target organ is the mammary gland (an inactive gland is shown here) which is regulated by MAMMOTROPHS, which are ACIDOPHILS in the anterior pituitary. Oxytocin from cell processes in the POSTERIOR PITUITARY stimulates the contraction of the myoepithelial cells of lactating mammary glands.
6. Match target organ 6
- Region A
- Cell type B
- Cell type C
- Cell type D
- NONE of the above
Answer
Correct answer 1., region A. The target organ is the kidney. Water permeability of the collecting ducts is regulated by ADH, which is released from cell processes in the POSTERIOR PITUITARY.
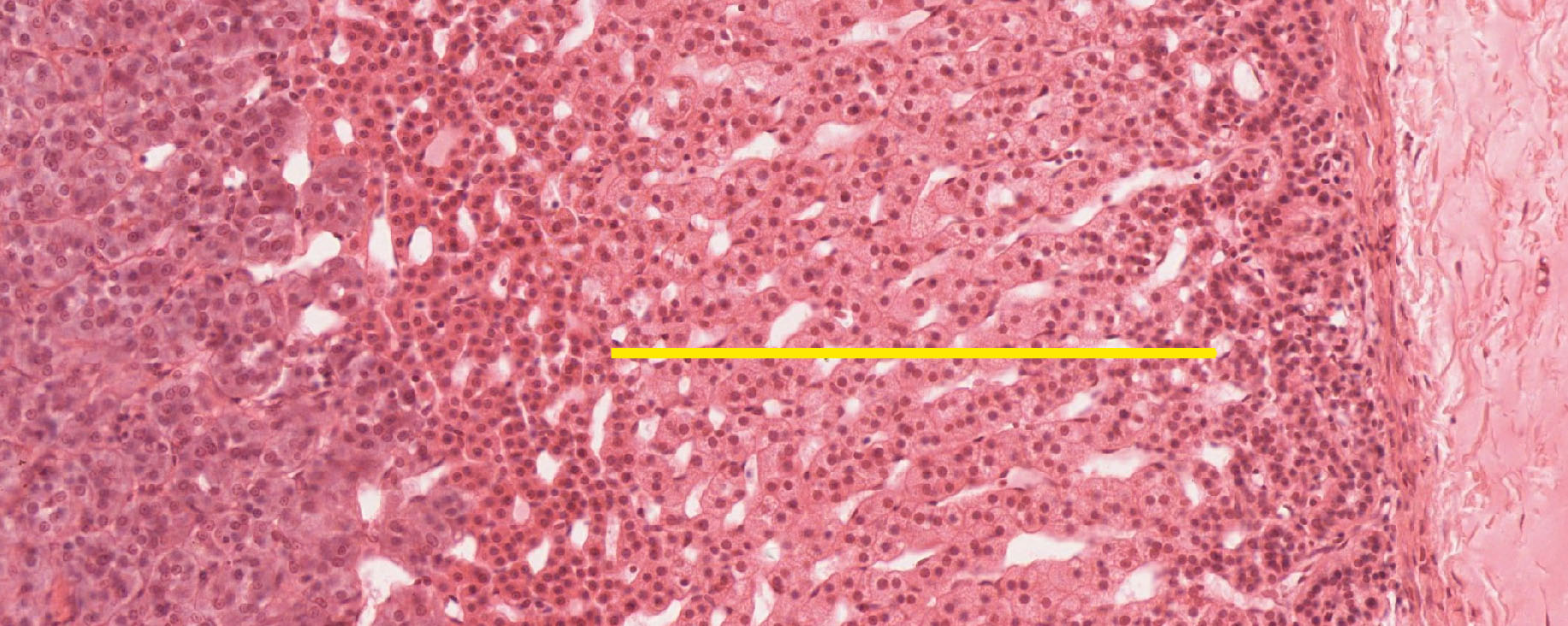
7. What would be the physiological result of HYPOactivity of the layer of cells within the bracket?
- Salt wasting due to insufficient production of mineralocorticoids (e.g., aldosterone).
- Addison's disease due to insufficient production of glucocorticoids (e.g., cortisol).
- HIGH blood calcium levels (hypercalcemia).
- LOW blood calcium levels (hypocalcemia).
- Low basal metabolic rate due to insufficient production of thyroxin (T4) and triiodothyronine (T3).
Answer
Correct answer 2. The cells indicated are in the zona fasciculata of the adrenal gland and are the primary source of glucocorticoids. Choice 'A' refers to cells of the zonal glomerulosa cells. Choice 'C' refers to HYPERactivity of the parathyroid gland. Choice 'D' refers to HYPOactivity of the parathyroid gland. Choice 'E refers to follicular cells of the thyroid gland.
8. Cells in which region are producing epinephrine?
- A
- B
- C
- D
- NONE of the above
Answer
Correct answer 1. (A). Epinephrine is produced by cells of the adrenal medulla.
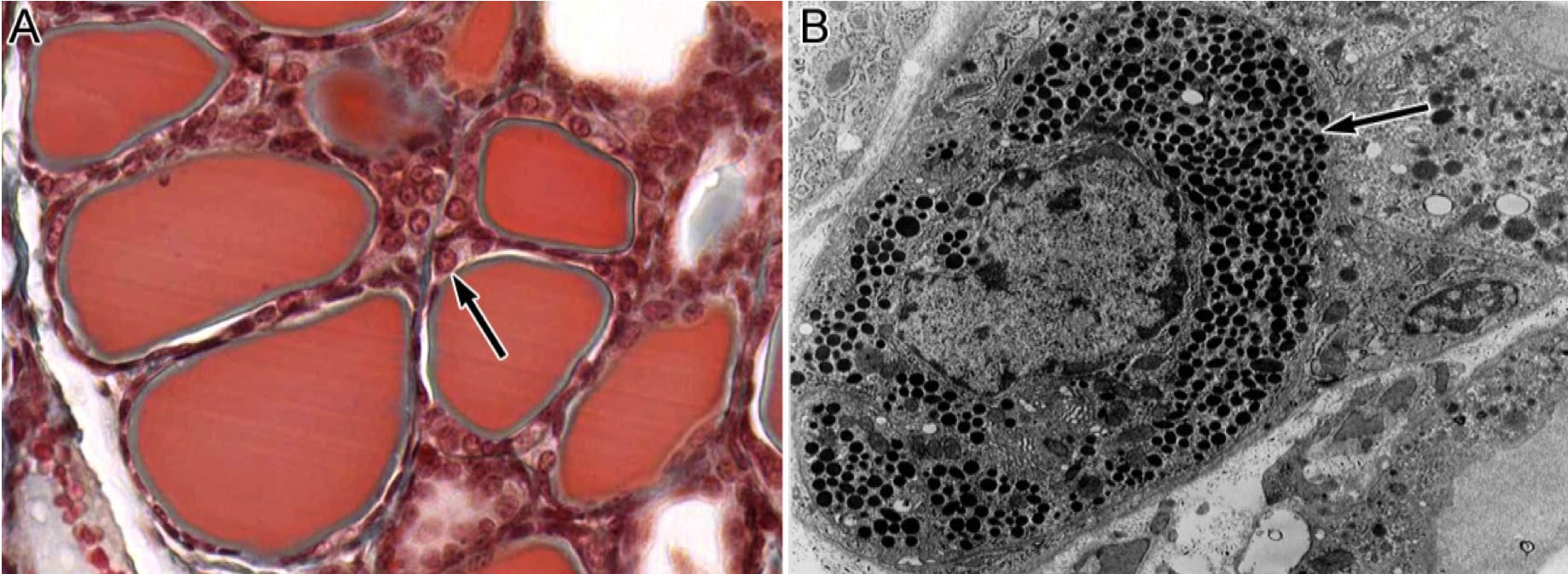
9. The cell indicated in the light micrograph in panel A and in the electron micrograph in panel B may secrete which of the following possible products?
- Thyroid hormone
- Thyroid stimulating hormone
- Calcitonin
- Parathyroid hormone
- Testosterone
- Epinephrine or norepinephrine
- Glucocorticoids
- Progesterone
Answer
Correct answer 3., calcitonin. The cell indicated is a parafollicular or C-cell of the thyroid gland. The tissue in panel A is a bit abnormal in that it has been made HYPOACTIVE by a hypophysectomy. Without TSH produced by thyrotropes of the anterior pituitary, the thyroid follicular cells become flattened. The C-cells are not affected, however, and they remain the same size, making them easier to spot in and around the follicles.
10. Hypothyroidism may be caused by malfunction of which cell type shown in this drawing of the anterior pituitary?
- A
- B
- C
- D
- E
Answer
Correct answer 4. (D). Malfunction of thyrotropes, which are basophils, in the anterior pituitary may be one cause (although VERY rare) of hypothyroidism.