- Be able to identify principal layers of the skin (epidermis, dermis and hypodermis) at the light microscope level and know the principal functions of each layer.
- Be able to identify the layers of the epidermis in thick and thin skin and describe the major cellular events that take place in each layer in the process of keratinization.
- Identify melanocytes and explain the process of pigment formation in the skin.
- Be able to recognize Meissner's and Pacinian corpuscles.
- Be able to identify eccrine and apocrine sweat glands, as well as sebaceous glands at the light microscope level.
- Identify the components of the pilosebaceous apparatus and know the structural and developmental relationship between each component and the epidermis of the skin.
The skin and its associated structures, hair, sweat glands and nails make up the integumentary system.
A. Thick skin
Slide 106 thick skin, sole of foot H&E View Virtual Slide
Slide 112 thick skin, sole of foot H&E View Virtual Slide
Slide 112N thick skin, sole of foot H&E View Virtual Slide
In this slide the structure of skin, especially the epidermis, is exaggerated in response to the continued stress and abrasion applied to the plantar surface of the foot. Study the epidermis in slides 106, 112, and 112N. Identify the various strata:
- Stratum basale (also known as S. germinativum): A single layer of cuboidal to columnar cells resting on and separated from the underlying dermis by a basal lamina. Mitotic figures occur in this layer.
- Stratum spinosum: Several layers in thickness. In reduced light, the cells appear interconnected by "spinous" processes.
- Stratum granulosum: A few layers of cells that are characterized by numerous, dense, basophilic granules. These are keratohyaline and membrane coating granules.
- Stratum corneum: Note the striking change in cellular morphology. The cells are flattened, devoid of nuclei or cytoplasmic granules, and filled with mature keratin (slide 112N). In slides 106 or 112, however, nuclei are still present in many cells of this layer, which are not normal. Because of differential dye penetration, the staining of the stratum corneum is variable and unpredictable. Sectioning artifacts are common.
The principal cell type of the epidermis is termed a keratinocyte and you will see this term used as a general descriptor for the epithelial cell found in any stratified squamous epithelium. Note the absence of blood vessels in the epidermis. Nourishment is obtained by diffusion from capillaries in the underlying dermis. The interface of the epidermis and dermis is uneven. A pattern of ridges and grooves on the deep surface of the epidermis fit a complementary pattern of corrugations of the underlying dermis. The projections of the dermis are called dermal papillae and those of the epidermis, epidermal ridges (pegs), because of their appearance in vertical sections of the skin. However, these terms are not always accurately descriptive of the three dimensional configuration of the region of interdigitation. With low power, identify the epidermal ridges and dermal papillae. What is the function of the epidermal ridges and dermal papillae
Answer
Epidermal ridges and dermal papillae provide increased surface area for the epidermis and dermis to connect.
Note the finer arrangement of collagen fibers in the papillary dermis slide 112N papillary dermis View Image as opposed to that of the reticular dermis slide 112N reticular dermis View Image (refer back to slide 033 morphology and distribution of elastic fibers View Image in order to review the morphology and distribution of elastic fibers in the dermis). The fatty layer beneath the dermis, the subcutaneous connective tissue, is often called thehypodermis or superficial fascia. It is this layer that allows the skin to "move".
B. Thin Skin
Slide 105-1 hair follicle H&E View Virtual Slide
Slide 105-2 thin skin H&E View Virtual Slide
Slide 104-1 thin skin H&E View Virtual Slide
Slide 104-2 thin skin H&E View Virtual Slide
The epidermis in thin skin is much thinner and simpler in structure. Each stratum is thinner and the stratum granulosum may be absent. Melanocytes #105-1 melanocytes View Image (derived from neural crest cells) capable of producing the pigment melanin are numerous in the deeper (toward the base) layers of the epidermis. They can be identified by the presence of a nucleus surrounded by a clear space. The cells with brownish pigments are actually keratinocytes that have received melanin granules from the melanocytes by pigment donation. The slides 104-1 and 104-2 are skin samples from lighter and darker skinned individuals. It is not difficult to tell which sample is from which individual. Note the presence of portions of hair follicles and sebaceous glands in the dermis.
A. Meissner's Corpuscles
Slide UCSF 180 finger tip H&E View Virtual Slide (virtual slide courtesy of the University of California, San Francisco)
Look at slide 112 thick skin, sole of foot H&E View Virtual Slide (note, there's only one corpuscle apparent in this slide) Meissner's corpuscles. Slide UCSF 180 Meissner's corpuscles View Image are touch receptors that are responsive to low-frequency stimuli and are usually associated with hairless skin of the lips and palmar and plantar surfaces, particularly those of the fingers and toes. Generally, these receptors are tapered cylinders located in the undulating connective tissue just underneath the stratified epithelium of the skin. The long axis of the cylinder is perpendicular to that of the overlying epidermis and is usually about 150 um long and is usually tucked within extensions of the underlying connective tissue dermis (called "dermal papillae") that project into the underside of the epidermis. Within these receptors, one or two nonmyelinated endings of myelinated nerve fibers follow a spiral path through the corpuscle. The fibers are accompanied by ensheathing Schwann cells, the nuclei of which are flattened and stacked on top of each other giving the corpuscle its characteristic irregular, lamellar appearance.
B. Pacinian Corpuscles
Slide 108 Fetal fingar H&E, 20X View Virtual Slide
Slide 108-1 Fetal fingar Masson View Virtual Slide
Slide 042 Mesentery H&E View Virtual Slide
Slide 095 Small arteries and vein H&E View Virtual Slide
Slide 095M Mesentary Masson View Virtual Slide
Pacinian corpuscles slide 095M View Image (best seen in slide 108-1) are large, ovoid structures up to 1 mm in diameter found in the dermis and hypodermis of the skin and also in the connective tissue associated with bones, joints, and internal organs. They respond primarily to pressure and vibration and are composed of a myelinated nerve ending surrounded by a capsule. The nerve enters the capsule at one pole (which might be out of the plane of section and therefore not visible) with its myelin sheath intact but then it is quickly lost. The unmyelinated portion of the axon extends toward the opposite pole from which it entered and its length is covered by flattened Schwann cell lamellae that form the inner core of the corpuscle. The remaining bulk of the capsule, or outer core, is comprised of a series of concentric, onionlike lamellae with each layer separated by an extracellular fluid similar to lymph. Each lamella is composed of flattened Schwann cells and endoneurial fibroblasts. In addition the fluid between each layer, delicate collagen fibers may be present as well as occasional capillaries. Displacement of the lamellae by pressure or vibrations effectively causes depolarization of the axon, which sends the signal to the central nervous system.
Slide 107 Scalp hair H&E View Virtual Slide
Underneath the thin epidermis, there are numerous circular to oblong structures with a hollow or yellow-brown center and surrounding cellular layers. These structures are hair follicles slide 107 View Image sectioned transversely or tangentially at different levels. The keratinized component of the hair occupies the central cavity of the follicle, and appears yellow-brown when present. However, the hair often falls out during tissue processing, in which case the central cavity will appear to be occupied by just empty space. The surrounding layers of clear cells form the external root sheath of the hair, which is a downgrowth of the epidermis. In fact, in cases where most of the epidermis is removed (such as severe abrasions or when taking skin graft), it is cells of the external root sheath that will divide and spread over the exposed surface to re-establish the epidermis. In some sections, you may also see an internal root sheath of darker staining cells right up against the hair follicle - this is the layer of cells that actually produce the keratinized hair shaft. Note also the presence of sebaceous glands slide 107 View Image and the arrector pili muscle slide 107 View Image near the hair follicle. In most instances, you will not find complete pilosebaceous units in a single section, so a bit of mental reconstruction will be required.
A. Eccrine sweat gland
Slide 106 Thick skin, sole of foot (Homo) View Virtual Slide
Slide 112 Thick skin (Homo) View Virtual Slide
Slide 112N Thick skin (Homo) View Virtual Slide
Slide 105-1 Thin skin (Homo) View Virtual Slide
Numerous coiled eccrine sweat glands are located at the junction of dermis and hypodermis. The coiled morphology can be particularly appreciated in the example shown in slide 112N. Distinguish between the secretory portions of the gland (secretory cells and myoepithelial cells; the latter are best seen in the apocrine gland, see below, slide 111 and 104-2) and the stratified (two layers) cuboidal epithelial cell-lined duct. Where do the ducts empty?
Answer
Ducts of eccrine sweat glands empty onto the surface of the skin. Apocrine glands, however, empty into hair follicles in the axillary, areolar and perianal regions.
How does sweat get to the surface?
Answer
Eccrine sweat glands have ducts that lead to the surface of the skin. Eccrine sweat glands are a type of merocrine gland (a gland that releases its product by exocytosis). The secretory cells of the eccrine gland are surrounded by myoepithelial cells which can contract to propel its secretions to the surface. Apocrine sweat glands (apocrine being a misnomer, they are truly a merocrine gland, not an apocrine gland) function in the same way, however, their ducts lead to hair follicles, not directly to the skin surface.
B. Apocrine glands
Slide 109-1 Perianal region Masson View Virtual Slide
Slide 109-2 Perianal region PAS/Pb hematoxylin View Virtual Slide
Slide 111 axilla, subcutaneal region Masson View Virtual Slide
Slide 104-2 View Virtual Slide [orientation] (this slide has both eccrine AND apocrine sweat glands; see if you can identify them)
Look in the deep dermis or hypodermis for secretory tubules with a wide lumen. The epithelium is cuboidal to columnar with distinct apical secretory granules. What should be apparent in your section is the apical "blebbing" of the secretory cells that was responsible for histologists originally designating these cells as "apocrine" secretory cells, although we now know the cells actually secrete in a MEROCRINE manner just like eccrine sweat glands. The "apocrine" sweat glands, present in the axillary, areolar, and anal regions, represent the second type of sweat glands. These glands produce a viscous secretion which acquires a distinctive odor as a result of bacterial decomposition. In complete transverse sections of the glands (e.g., slide 111), look for oblong nuclei just inside the basement membrane. These are the nuclei of myoepithelial cells. In some planes of section, the nuclei may appear round. Now look for a tangential section of the gland. Look for regularly spaced, elongate strands of cytoplasm investing the outside of the secretory epithelium. With a bit more looking you should be able to see that these elongate bits of cytoplasm contain the above mentioned oblong nuclei. Slide 104-2 is another good place to see myoepithelial cells slide 104-2 View Image; look for eosinophilic strands of cytoplasm and small nuclei just peripheral to the secretory epithelial cells. In PAS stained slides (e.g. slide 109-2), densely staining granules are obvious in the apical cytoplasm the secretory cells, but the cytoplasm of myoepithelial cells is not well seen. Instead you see darker pink-stained basement membrane between the projections of myoepithelial cells. The relatively great number of these cells in sweat glands (and mammary glands) can only be appreciated by studying such tangential cuts. Please also look for apocrine sweat gland ducts in these slides. They look similar to eccrine gland ducts described above (small diameter and small lumen with a stratified cuboidal epithelium). Similarly, they also lack lack myoepithelial cells. Make sure you can discriminate the ductal portion of apocrine sweat glands from their secretory portion.
65 Epidermis Skin View Virtual EM Slide
Review the layering of the epidermis. Remember that there is a continuous process of cell migration and differentiation from the basal cell layer to the most superficial layer. Review the features of the epidermal-dermal junction.
67 Epidermis - Details of the Stratum Spinosum View Virtual EM Slide
Observe the abundance of tonofibrils (= keratin intermediate filaments) and ribosomes and the small number of mitochondria. Note the absence of Golgi apparatus and granular endoplasmic reticulum. Epidermal cells do contain these organelles but in reduced amount, as the bulk of synthesis is for structural proteins, not exportable ones. What is the function of the numerous desmosomes? The function of the tonofibrils? (IN4)
69 Epidermis – Details of the Stratum Granulosum and Stratum Corneum View Virtual EM Slide
Note the keratohyaline granules in the cells of the stratum granulosum. The keratinization process is completed in the cell layers above the stratum granulosum, indicated by the disappearance of nuclei and cell organelles. Note that the cornified cells are of variable appearance (some "dark" and some "light") a reflection of the tissue processing rather than of a functional difference.
Click on a question to reveal the answer.
What is the function of the numerous myoepithelial cells (in sweat glands)?
Myoepithelial cells are what propel the secretory contents of the glands to the surface of the body.
What is the function of the epidermal ridges and dermal papillae?
Epidermal ridges and dermal papillae provide increased surface area for the epidermis and dermis to connect.
Where do the ducts empty?
Ducts of eccrine sweat glands empty onto the surface of the skin. Apocrine glands, however, empty into hair follicles in the axillary, areolar and perianal regions.
How does sweat get to the surface?
Eccrine sweat glands have ducts that lead to the surface of the skin. Eccrine sweat glands are a type of merocrine gland (a gland that releases its product by exocytosis). The secretory cells of the eccrine gland are surrounded by myoepithelial cells which can contract to propel its secretions to the surface. Apocrine sweat glands (apocrine being a misnomer, they are truly a merocrine gland, not an apocrine gland) function in the same way, however, their ducts lead to hair follicles, not directly to the skin surface.
What is the function of the numerous desmosomes (in the basal cell)? The function of the tonofibrils?
Desmosomes are spot junctions that serve to connect the individual cells of the epidermis to each other. These cells are also filled with keratin (intermediate) filaments called tonofibrils. They help provide the cell with strength and support and also insert into the desmosomes. Hemidesmosomes, on the other hand, serve to attach the epidermis to the dermis by connecting the cells of the stratum basale to the dermis via the basal lamina.
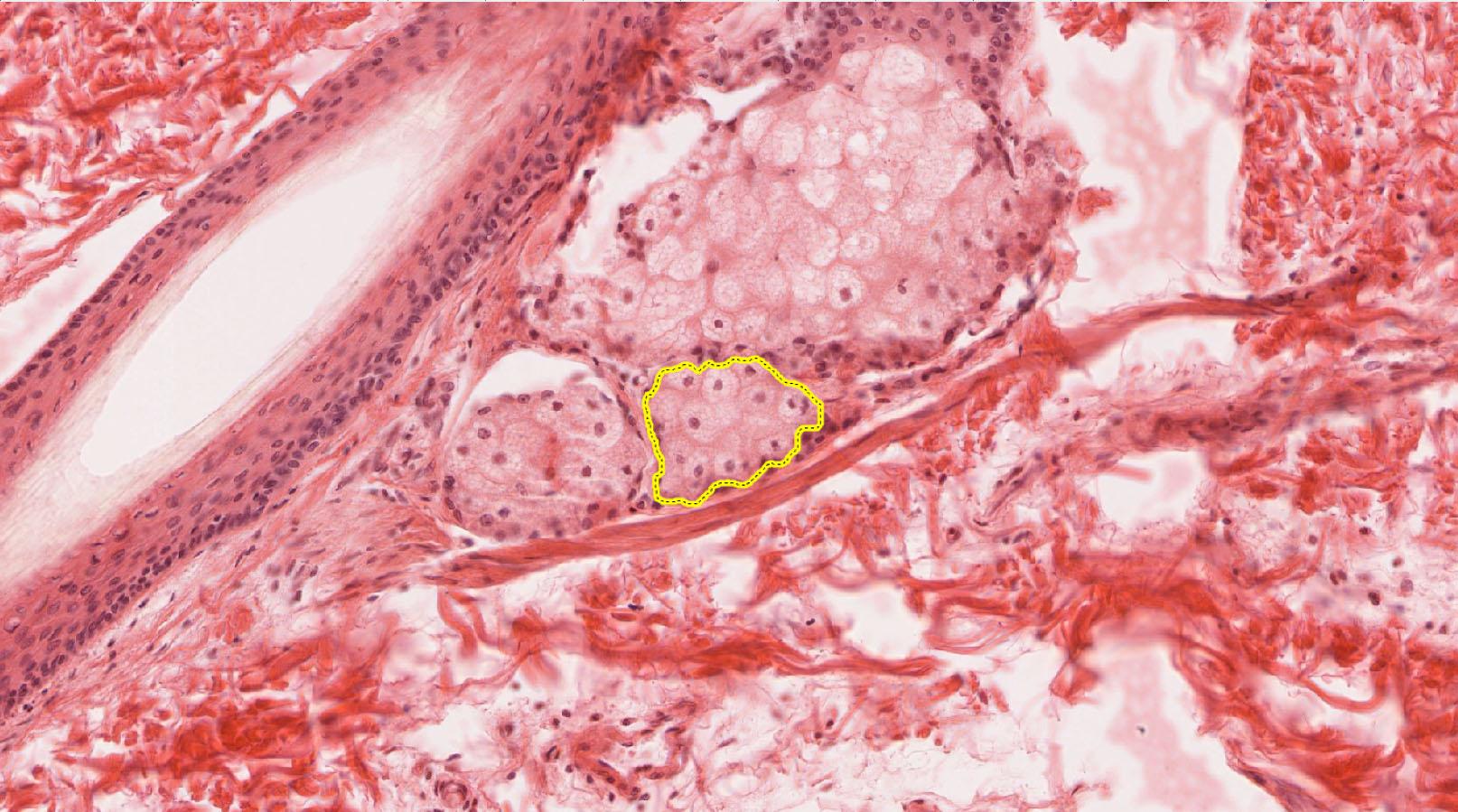
1. Identify the true statement(s) about the cluster of cells enclosed by the yellow outline on the slide.
- They produce ceramide.
- They secrete in an apocrine manner.
- The secrete in an eccrine (or merocrine) manner.
- All of the above statements are true.
- None of the above statements is true.
Answer
Correct answer 5. None of the above statements are true - the yellow outline encloses secretory cells of a SEBACEOUS gland. These cells secretes lipid-rich SEBUM by a HOLOCRINE mechanism.
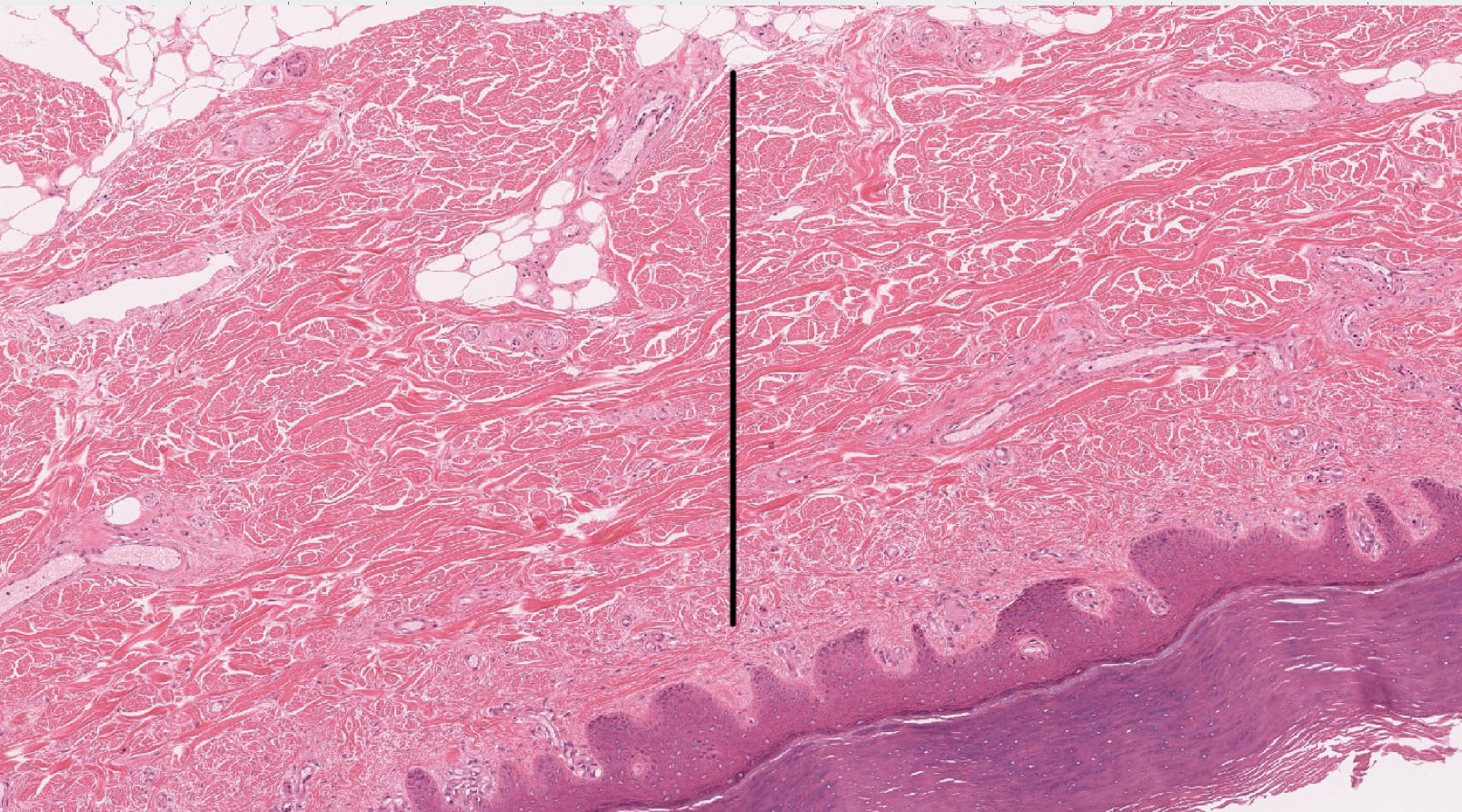
2. Identify the true statement(s) about the tissue layer indicated by the black line.
- It is where melanocytes usually reside.
- It contains cells densely packed with keratin tonofilaments.
- consists primarily of type III collagen fibers.
- consists primarily of type I collagen fibers.
- All of the above statements are true,
- None of the above statements are true.
Answer
Correct answer 4. This layer is the RETICULAR LAYER of the dermis and consists primarily of a coarse network of type I collagen fibers (which is why the term "reticular" is used here). Type III collagen is primarily found in the PAPILLARY layer of the dermis.
3. In which places/structures can myoepithelial cells be found?
- In active mammary gland acini
- In inactive mammary gland ducts
- In eccrine sweat gland acini
- In apocrine sweat gland acini
- In all of the above cellular structures
- In none of the above cellular structures
Answer
Correct answer 5. In all of the listed cellular structures (Answers 1 to 4). Myoepithelial cells are found in the acini and ducts of mammary glands and in the acini of eccrine and apocrine sweat glands. Note that they are NOT found in sebaceous glands (not needed since these glands secrete in a holocrine manner).
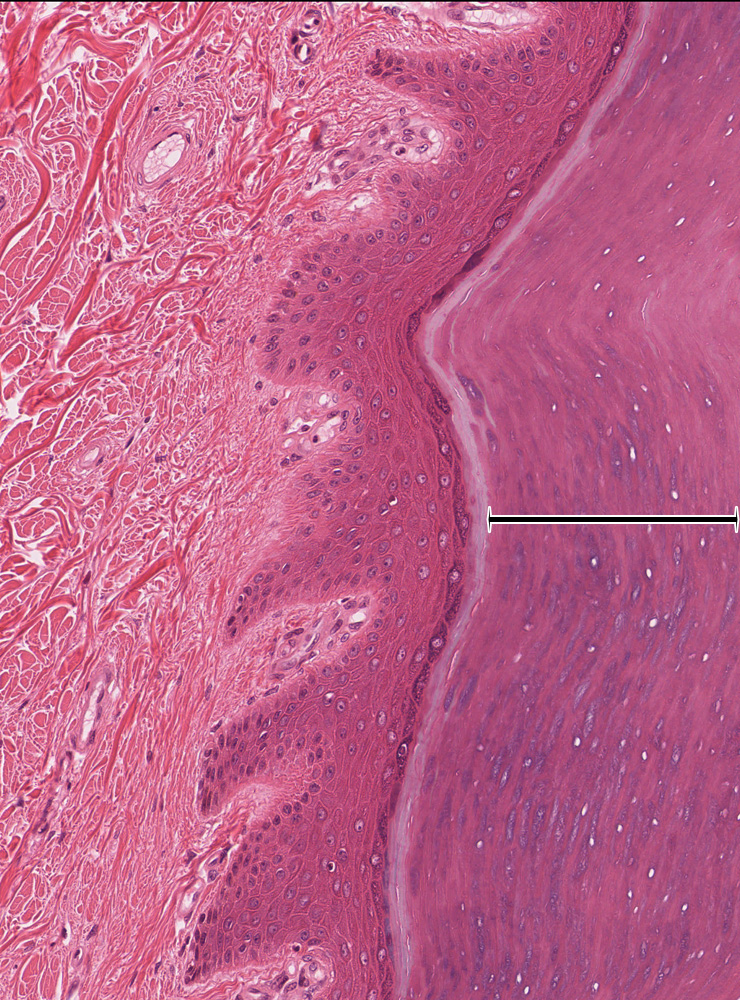
4. Identify the layer indicated by the black bracket.
- The reticular layer of the dermis
- The papillary layer of the dermis
- The stratum basale of the epidermis
- The stratum granulosum of the epidermis
- The stratum corneum of the epidermis
Answer
Correct answer 5. The bracket indicates the STRATUM CORNEUM of the epidermis.
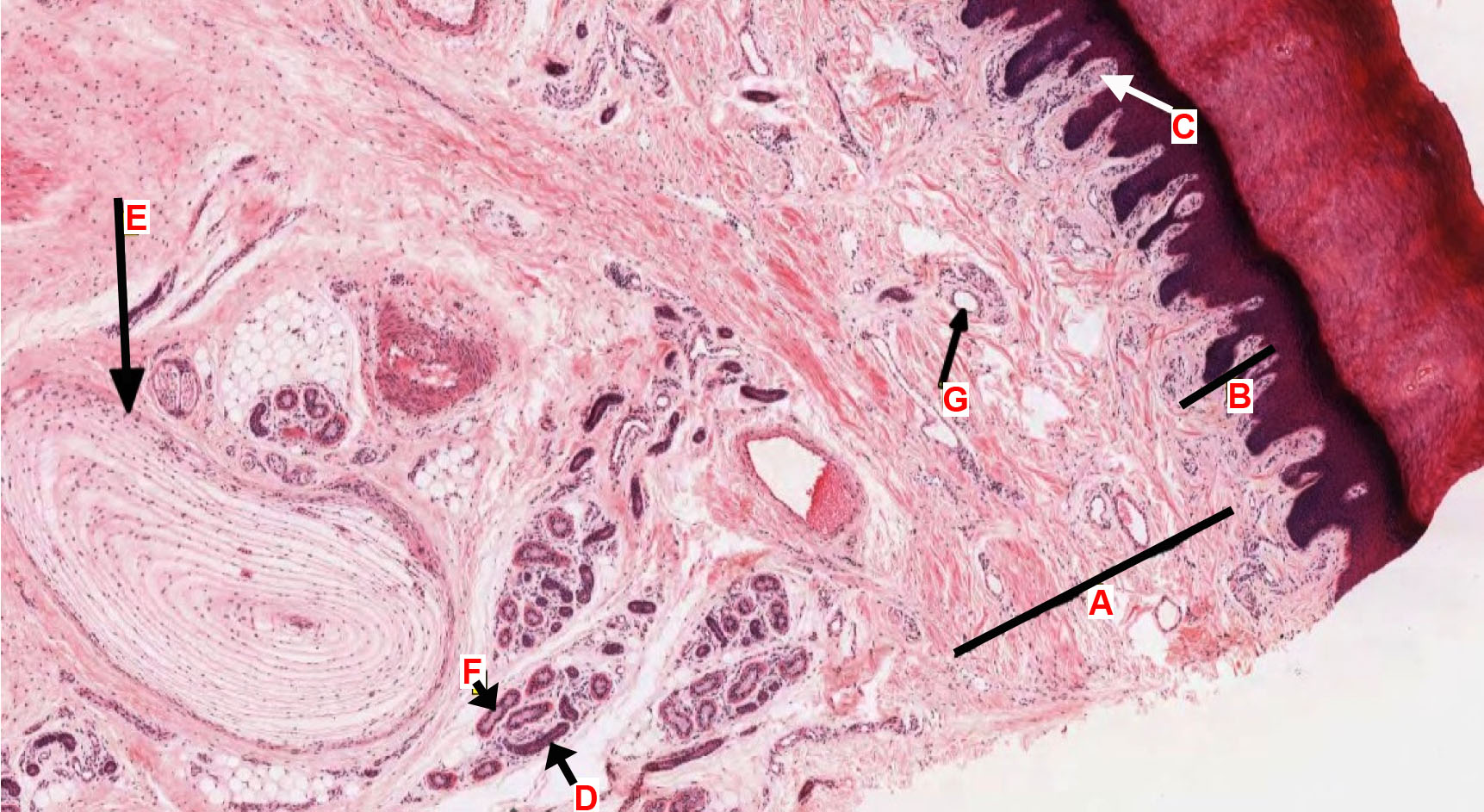
5. Match the text descriptions below with the appropriately feature that is labeled by a letter in the tissue section. Some labeled features may be referred to once, more than once, or not at all. If the description refers to something NOT labeled on the slide, answer "NONE."
Note: there won't be a matching question like this on the exam, but the overall content is helpful for review.
- Reticular dermis
- Which structure(s) respond(s) to light touch and low frequency stimuli
- An eccrine sweat gland duct
- Which structure(s) is/are innervated by a neuron, whose cell body is in a dorsal root/sensory ganglion
- An apocrine sweat gland secretory acinus
Correct Answers:
1. Letter A labels the reticular dermis, so named because of the network of coarse, type I collagen fibers (Letter B indicates the papillary dermis).
2. Letter C labels Meissner's corpuscles, which are mechanosensory receptors that respond primarily to light touch and low frequency stimuli.
3. Letter D labels the ductal portions of sweat glands that are lined with a stratified cuboidal epithelium consisting of small, darkly staining cells. It is most likely an eccrine sweat gland duct given its proximity to a nearby acinus ('F') which is clearly eccrine (based on the small lumen).
4. Letters C AND E label both Meissner's AND Pacinian corpuscles, which are sensory receptors that are innervated by myelinated axons of dorsal root ganglion cells.
5. NONE of the letters labels an apocrine sweat glands as none is present in this tissue section ('G' is a venule).