- Recognize male germ cells at different steps of spermatogenesis in the seminiferous tubules, and explain which steps involve mitosis or meiosis, and which involve cellular differentiation into sperm (spermiogenesis).
- Recognize Sertoli and Leydig cells and explain their roles in the production of sperm and the regulation of the male reproductive system.
- Know the structural organization and functional parts of spermatozoa.
- Recognize the various parts of the male reproductive tract in histological sections (seminiferous tubules, rete testis, efferent ducts, epididymis, ductus/vas deferens), and explain their contributions in the production of semen and during ejaculation.
- Recognize and understand the histological organization and function of seminal vesicles and the prostate gland.
- Recognize and understand the histological organization of the penis and know the role of its components in erection and detumescence.
Slide 270 testis testis H&E View Virtual Slide [see orientation]
Slide 270ex testis H&E View Virtual Slide [see orientation]
Slide 275 Testis H&E View Virtual Slide [see orientation]
Slide UCSF 363 testis View Virtual Slide (virtual slide courtesy of the University of California, San Francisco)
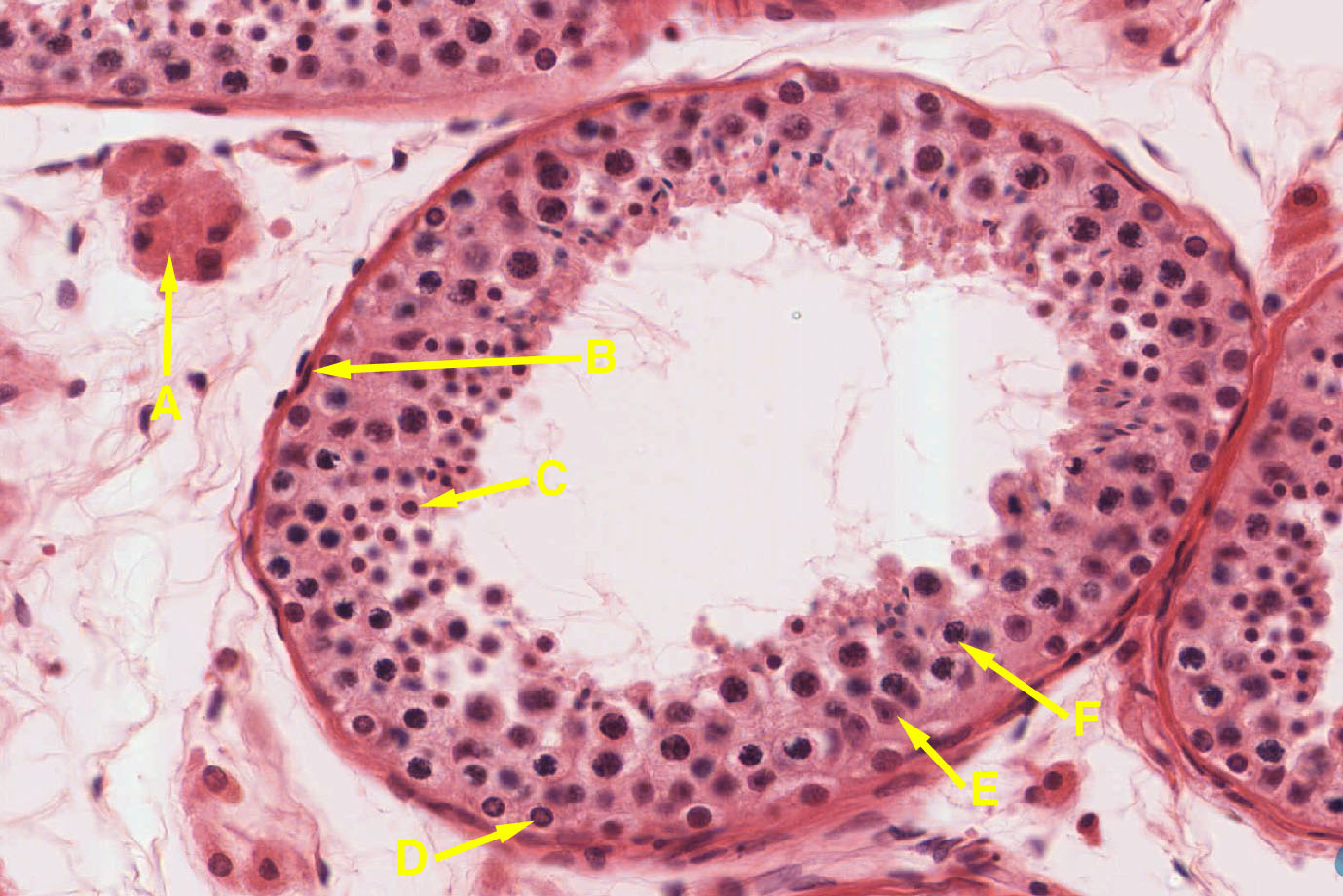
Slide 273 Testis H&E immature View Virtual Slide
These slides (except for the UCSF slide) include both testis and epididymis (you will study epididymis later in this laboratory session): the testis is the larger of the two structures on the slide. The capsule of the testis is composed of dense connective tissue and is called thetunica albuginea. Within the testis you will see numerous profiles of seminiferous tubules, with interstitial tissue between them. In the interstitial tissue between the seminiferous tubules are clusters of Leydig cells, which secrete the male steroid hormone, testosterone. These are the most prominent cells in the interstitial tissue, but in slide 270 of some slide sets, the Leydig cells slide 270 View Image are not seen very clearly (in that case, see them in slide 275 View Image). Also visible in the interstitial tissue are blood vessels and smaller cells characteristic of loose connective tissue. Now take a closer look at the the seminiferous tubules in slide 270 View Image [Orientation] (in some of the seminiferous tubules the epithelium may be pulled away somewhat from the basement membrane, leaving a white space, which is an artifact). Each seminiferous tubule is surrounded by a boundary layer or tunica propria, composed of flattened cells, several cells thick. Most of the cells that lie against the basement membrane and have round nuclei are spermatogonia. Don’t worry about distinguishing between type A and type B spermatogonia. Now look for considerably larger nuclei midway up in the epithelium that are also round and are filled with a tangle of dense chromosomes. These are the nuclei of relatively mature primary spermatocytes, which are in the extended prophase of the first meiotic division. These are numerous but unfortunately not always well preserved (the nuclei may be somewhat swollen or distorted). All of the smaller cells in the upper half of the epithelium (toward the lumen of the tubule) are spermatids in various stages of differentiation into mature sperm. The spermatids initially have round nuclei, but these gradually become smaller, denser and assume the shape of sperm heads. The smallest black structures you see are the heads of mature spermatids about to be released into the lumen. Their tails are difficult to make out. Now look for Sertoli cell nuclei, which are large, relatively pale and irregular in shape, and contain a prominent nucleolus (sometimes out of the plane of section). Their nuclei commonly occur just above (toward the lumen from) the spermatogonia. Secondary spermatocytes are rarely seen, since almost immediately after they arise they undergo the second meiotic division to become spermatids. If you are anxious to see secondary spermatocytes, find division figures and look around them for nuclei that are intermediate in size between those of primary spermatocytes and spermatids. They are hard to find, so don’t spend much time looking.
Answer
With so many types of cells in such a small space, sometimes it is hard to tell the difference among these types of cells. Sertoli cells envelop the gamete throughout the process of development. Sertoli cells can be distinguished because they have a pale, oval-shaped nucleus with a prominent nucleolus. The nucleus is generally located midway through the cell, however, due to the plane of section, it can appear to be anywhere along the wall of the tubule. Spermatogonia are large precursor cells and are always located along the basement membrane of the tubule. Primary spermatocytes have large, heterochromatic nuclei, and they are located between the basement membrane and the lumen of the tubule. Occasionally mitotic figures can be seen in them. They do not have nucleoli.
Slide 273, obtained from a pre-adolescent, shows what the testis looks like before puberty. The seminiferous tubules slide 273 View Image contain mostly Sertoli cells (oval nuclei) and spermatogonia (round nuclei), although there may be an occasional primary spermatocyte. Most of the cells in the interstitial tissue between the tubules are fibroblasts, and there are few, if any, differentiated Leydig cells.
Slide 270 testis testis H&E View Virtual Slide [see orientation]
Slide 270ex testis H&E View Virtual Slide [see orientation]
Slide 275 Testis H&E View Virtual Slide [see orientation]
Returning to the slides of the seminiferous tubules, study the passageway by which the sperm pass from the seminiferous tubules through the rete testis, efferent ducts and epididymis to reach the tail of the epididymis, where they are stored in preparation for an ejaculation. Scan along the tunica albuginea of the testis, looking for a region where it thickens and is permeated by a network of flattened channels in the dense connective tissue. This portion of the testis is known as the mediastinum; the network of channels is the rete testis and is probably best seen in slide 270 View Image or slide 275 View Image Observe that the rete testis is lined with a cuboidal (or sometimes low-columnar) epithelium and you may see occasional microvilli. (Purely as an aside, these cells also have a single or "primary" cilium. Obviously, these cilia don't contribute much in the way of helping to propel sperm through the channel. Instead, they may function as chemoreceptors allowing the lining cells to monitor and modify the luminal contents). The sperm leave the testis by means of these channels to reach the efferent ducts. However, for now, shift your attention outside the testis to the part of the epididymis that is included in this slide. You will see numerous sections through the long and convoluted duct that makes up the epididymis apparent in slide 275 View Image and slide 270 View Image. The epithelium of the duct is pseudostratified columnar. The tall epithelial cells have long microvilli on their apical surface (sometimes called “stereocilia”, although they are not cilia at all). You may be able to make out a thin layer of smooth muscle around the tubules, which presumably acts by peristalsis to move the sperm along. Now scan over the section looking for tubules of the efferent ducts, which connects the rete testis to the epididymal duct. The efferent duct tubules are often (but not always) smaller than epididymal tubules, and their epithelium varies considerably in height, giving the tubule lumen a characteristic irregular or "star" shape. The epithelium is generally simple columnar, and consists of two cell types, taller cells have with cilia and shorter cells without cilia. The efferent duct is the only portion of the male tract displaying true, motile, cilia. These tubules may also have a thin layer of smooth muscle around them. Efferent ducts are best demonstrated in slide 275 View Image, although slide 270 View Image shows a small region of efferent ducts amongst the epididymis.
Slide 284 20X spermatic cord H&E View Virtual Slide
This is a cross section through a spermatic cord, such as you will see in the gross anatomy laboratory. On one side of the section you will see a cross section of the ductus (or vas) deferens slide 284 View Image, which has a circular lumen, lined by a pseudostratified epithelium and surrounded by a very thick wall of smooth muscle. Elsewhere you will see sections through two or more branches of the testicular artery, surrounded by connective tissue that contains numerous veins of the pampiniform plexus slide 284 View Image (the veins are rather flattened and contain dark red blood). What is the function of the pampiniform plexus?
Answer
Sperm cannot develop if the testis is at body temperature. The pampiniform plexus helps to regulate testicular temperature, allowing sperm maturation. The plexus surrounds the testicular arteries and works as a countercurrent heat-exchange system to cool the arterial blood before it enters the testis. Along with the pampiniform plexus of veins, temperature in the testis is controlled by sweat glands on the scrotum and by the cremaster muscle, which controls the proximity of the testis to the body.
The testicular artery has a typical internal elastic membrane and prominent circular smooth muscle coat (comprising the tunica media). The veins of the pampiniform plexus lack the internal elastic membrane, and their walls are somewhat less muscular. The blood in the vessels may have black particles in it, an artifact of the fixation procedure. The association of the veins of the pampiniform plexus with the testicular artery constitutes a countercurrent exchange system to cool the blood somewhat on its way to the testis. In the connective tissue you will find nerves and, around the periphery of the section, some cross-sectioned bundles of smooth (dartos) slide 284 View Image and skeletal (cremaster) muscle slide 284 View Image .
Slide 075 seminal vesicle H&E View Virtual Slide
Slide 279 seminal vesicle H&E View Virtual Slide
These are cross sections through a seminal vesicle, which you may remember from gross anatomy is a rather sacculated and contorted tube (slide 75 is also the slide we used to study parasympathetic ganglia, which are readily observable in the wall of this organ). Study the section with your light microscope, noting the moderately-abundant smooth muscle in the wall. The epithelium of this gland lies on the surface of interconnecting mucosal folds that extend into the lumen from the muscular wall. The sparse connective tissue within the folds constitutes the lamina propria of this mucosa. The epithelium, which may be either simple columnar or pseudostratified columnar, produces a secretion (including fructose, ascorbic acid and other components) which is expelled from the gland by contraction of the muscular wall during ejaculation, constituting about 50-80% of the semen.
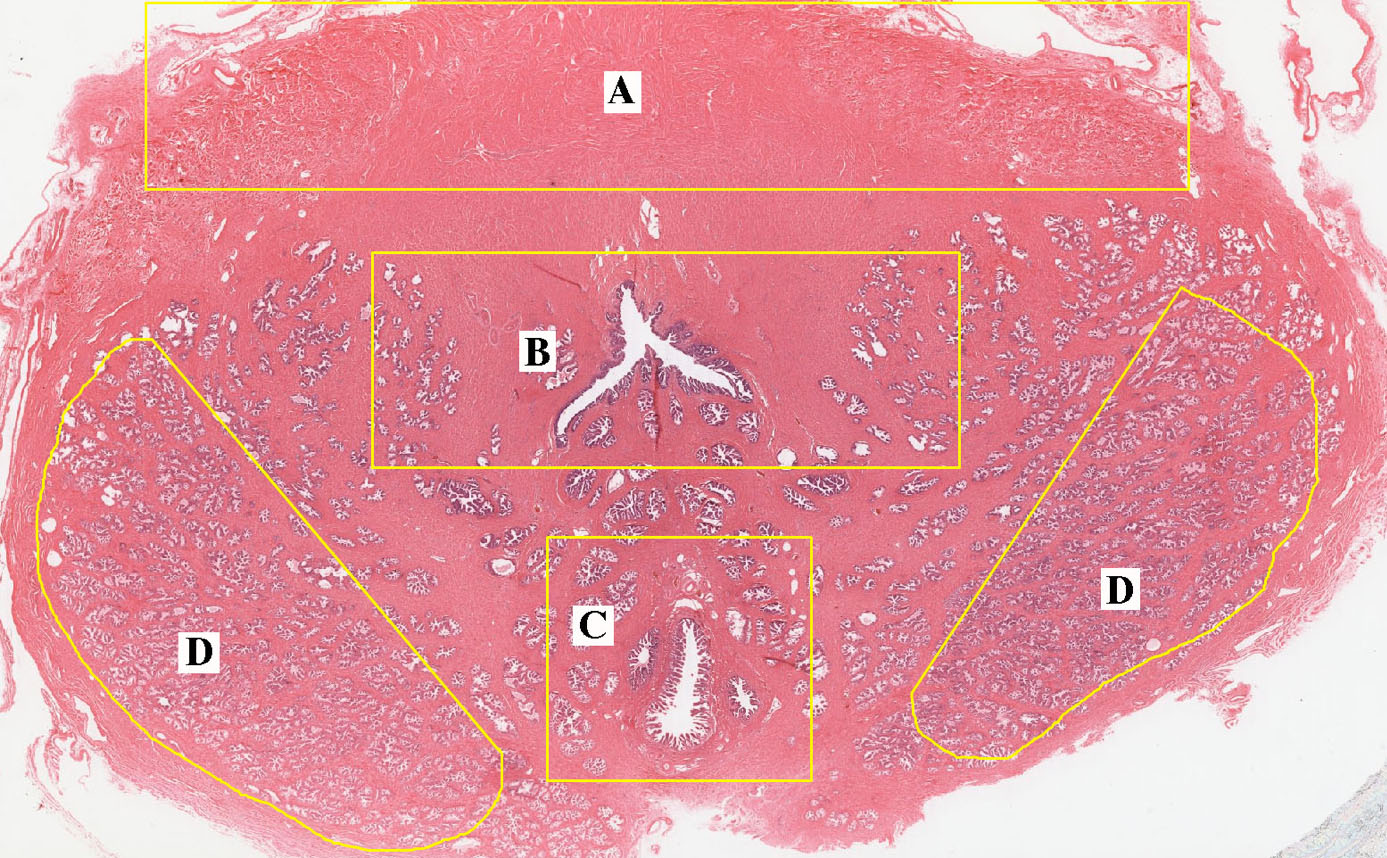
Slide 281 prostate H&E View Virtual Slide [see orientation]
Slide 281lex prostate Masson View Virtual Slide
Slide 282 prostate senile H&E View Virtual Slide
The prostate in an adult man is about the size and shape of a chestnut and contains 15-30 tubuloalveolar glands that empty separately into the prostatic urethra. The most important structures to see on the slide are the prostatic glands that are present over most of the section. The glands are embedded in a connective tissue that includes abundant smooth muscle, best appreciated in the trichome-stained section slide 281-EX View Image (recall that collagen fibers will stain blue-green whereas smooth muscle is pink with deep red nuclei), which produces the pulsations of the prostate that expel the content of the glands during ejaculation. The epithelium of the glands is simple columnar (there may be a few basal cells), and the cells differ greatly in height to give the epithelium a folded appearance. The epithelial cells secrete various components of the semen (including citric acid and acid phosphatase). In older individuals, there may be concretions (amyloid bodies) in the lumen of the glands, which are better seen in slide 282 View Image - the concretions are of little functional consequence, but they can be a helpful for the purposes of identifying the tissue. The prostatic urethra is present in the slide 281 prostate H&E View Image (it has a stratified epithelium several cells thick and numerous mucosal glands). Also present on slide 281 is the utricle flanked by paired ejaculatory ducts slide 281 prostate H&E View Image. With these landmarks, one can identify the various zones of the prostate that are clinically relevant in their propensity to become hyperplastic and/or cancerous:
- The peripheral zone slide 281 prostate H&E View Image contains the main glands located posterio-laterally in the outer parenchyma of the gland and is the site most susceptible to inflammation (prostatitis) and malignant neoplasia (prostatic carcinoma).
- The central zone slide 281 prostate H&E View Image is the region surrounding the utricle and ejaculatory ducts. Interestingly, this zone is relatively resistant to inflammation and hyperplasia.
- The transitional and periurethral zones slide 281 prostate H&E View Image surrounds the prostatic urethra and contains submucosal and mucosal glands that undergo non-cancerous proliferation, leading to benign prostatic hypertrophy (BPH), a condition that effects almost all males to some extent by age 80. Typically, the submucosal glands undergo hypertrophy first followed by the mucosal glands as the condition progresses.
- The anterior fibromuscular stroma slide 281 prostate H&E View Image is located anteriorly and contains no glandular tissue so it typically does not become hyperplastic.
Slide 286 penis H&E cross View Virtual Slide [see orientation]
This is a cross section through the shaft of the penis. Identify the two pale corpora cavernosa in slide 286 penis H&E cross View Image (occupying most of the central part of the section; the partition between the two may be incomplete), surrounded closely by a thick layer of dense connective tissue (pink), the tunica albuginea. Also observe the corpus spongiosum in the slide 286 penis H&E cross View Image, situated ventromedially and containing the slit-like penile urethra. Study the erectile tissue of the corpora cavernosa with your microscope, noting the connective tissue trabeculae and smooth muscle strands, as well as small blood vessels and nerves. The arterioles within the trabeculae are called helicine arteries(oles) slide 286 View Image because in the flaccid penis they are rather twisted (like a helix). Between the trabeculae are the venous sinuses, lined with endothelium. In the flaccid penis, the smooth muscle in the trabeculae and arterioles is under tonic contraction, limiting the entry of blood into the sinuses. Erection involves a relaxation of the smooth muscle of the arterioles (so more blood enters) and of the trabeculae (permitting the sinuses to expand freely), as well as a closing down of venous outflow due to compression of the veins that drain the erectile tissue (the veins draining the tissue are pushed up against the rigid connective tissue of the tunica albuginea when the erectile tissue swells). The organ expands by hydraulic pressure, and the shape of the erect penis is determined by the tunica albuginea. A resumed contraction of the smooth muscle in the helicine arterioles leads to detumescence. In each corpus cavernosum, note one or two arteries, the deep arteries slide 286 View Image, that supply the arterioles. If you look on the upper surface of the tunica albuginea, you will see the abundant nerve bundles that supply this organ.
258 Testis - Seminiferous Tubule View Virtual EM Slide
In this electron micrograph, showing a seminiferous tubule and adjacent interstitial tissue, you can see in more detail the same structures you have been viewing with the light microscope. In the seminiferous tubule, the large, round nuclei belong to more mature primary spermatocytes. Toward the lumen from these are the nuclei of spermatids. Note the occasional Sertoli cell nuclei and try to follow the extensive Sertoli cell cytoplasm as it passes up to enfold the spermatocytes and spermatids. In the interstitial tissue, observe the Leydig cells and capillaries (the latter are somewhat swollen because the testis was fixed for electron microscopy by perfusion of the fixative through the blood vessels).
259 Testis - Seminiferous Epithelium View Virtual EM Slide
This electron micrograph shows the seminiferous epithelium at a higher power than the previous electron micrograph (EM #258). Note the different appearances of the cell nuclei in spermatogonia, primary spermatocytes, Sertoli cells and spermatids.
262 Testis - Interstitial tissue View Virtual EM Slide
Clearly visible are a number of Leydig cells in the interstitial tissue of the testis. Also note a postcapillary venule, a capillary and lymphatic spaces.
264 Epididymis - Pseudostratified Columnar Epithelium View Virtual EM Slide
Tall cells of uniform height extend to the lumen, while short basal cells are limited to the base of the tubule. Note most of the stereocilia are transversely sectioned.
Click on a question to reveal the answer.
How can you differentiate between Sertoli cells, spermatogonia, and primary spermatocytes?
With so many types of cells in such a small space, sometimes it is hard to tell the difference among these types of cells. Sertoli cells envelop the gamete throughout the process of development. Sertoli cells can be distinguished because they have a pale, oval-shaped nucleus with a prominent nucleolus. The nucleus is generally located midway through the cell, however, due to the plane of section, it can appear to be anywhere along the wall of the tubule. Spermatogonia are large precursor cells and are always located along the basement membrane of the tubule. Primary spermatocytes have large, heterochromatic nuclei, and they are located between the basement membrane and the lumen of the tubule. Occasionally mitotic figures can be seen in them. They do not have nucleoli.
What is the function of the pampiniform plexus?
Sperm cannot develop if the testis is at body temperature. The pampiniform plexus helps to regulate testicular temperature, allowing sperm maturation. The plexus surrounds the testicular arteries and works as a countercurrent heat-exchange system to cool the arterial blood before it enters the testis. Along with the pampiniform plexus of veins, temperature in the testis is controlled by sweat glands on the scrotum and by the cremaster muscle, which controls the proximity of the testis to the body.
1. Which yellow arrow/letter marks diploid cells with 2N chromosomal number (hint: there are multiple answers)?
- A
- B
- C
- D
- E
- F
- NONE of the above
Answer
Correct answers: A (Leydig cells), B (fibroblasts of connective tissue capsule), D (spermatogonia), E (Sertoli cells), and F(Primary spermatocytes) are all somatic, DIPLOID cells with 2N chromosome number (23 paternal chromosomes and 23 maternal chromosomes for a total of 46).
2. Which cell(s) marked by a yellow arrow/letter have luteinizing hormone (LH) receptors?
- A
- B
- C
- D
- E
- F
- NONE of the above
Answer
Correct answer 1. (A). Leydig cells have LH receptors. They respond to LH by secreting testosterone.
3. Which yellow arrow/letter(s) mark diploid cell with a 4N chromosomal number?
- A
- B
- C
- D
- E
- F
- NONE of the above
Answer
Correct answer 7., none of the above (there is no tetraploid cell among the marked cells). 3. (C) indicates an early spermatid which is haploid with a 1N chromosome number.
4. Which cell marked by a yellow arrow/letter secretes androgen binding protein (ABP)?
- A
- B
- C
- D
- E
- F
- NONE of the above
Answer
Correct answer 5. (E). Sertoli cells respond to FSH (via FSH receptors) from the pituitary and secrete ABP (as well as INHIBIN, which feeds back to the pituitary to DOWNREGULATE FSH production). Note that the 'androgen' (testosterone) comes from LEYDIG cells. Sertoli cells of the immature testis produce anti-Müllerian hormone, which is important during development to cause regression of the 'Müllerian' ducts that give rise to structures of the female reproductive tract such as the uterus and oviduct.
5. Which two segments of the male reproductive system are connector by the epididymis?
- Seminiferous tubules to rete testis
- Rete testis to efferent ducts
- Efferent ducts to ductus (vas) deferens
- Vas deferens to prostatic urethra
- Prostatic urethra to penile urethra
Answer
Correct answer 3., the efferent ducts to ductus (vas) deferens. Choice 1. describes the 'tubuli recti' or 'straight tubules'. Choice 2. describes a transition that occurs directly; i.e. sperm travel through the rete testis into the efferent ducts without going through any sort of named intermediate tubule system. Choice 4. describes the ejaculatory ducts that travel through the prostate. Choice 5. also describes a transition that occurs directly.
6. Benign prostatic hypertrophy/hyperplasia (BPH) typically affects the tissue of which area indicated?
- A
- B
- C
- D
Answer
Correct answer 2. (B) as BPH typically affects glands of the periurethral and transitional zones. Region 'A' marks the anterior fibromuscular stroma, which typically does not hypertrophy. Region 'C' marks the 'central zone' associated with the utricle and ejaculatory ducts --this zone also does not typically hypertrophy. Region 'D' marks the peripheral zone - prostatitis (inflammation) and prostatic carcinoma typically occur in this region.
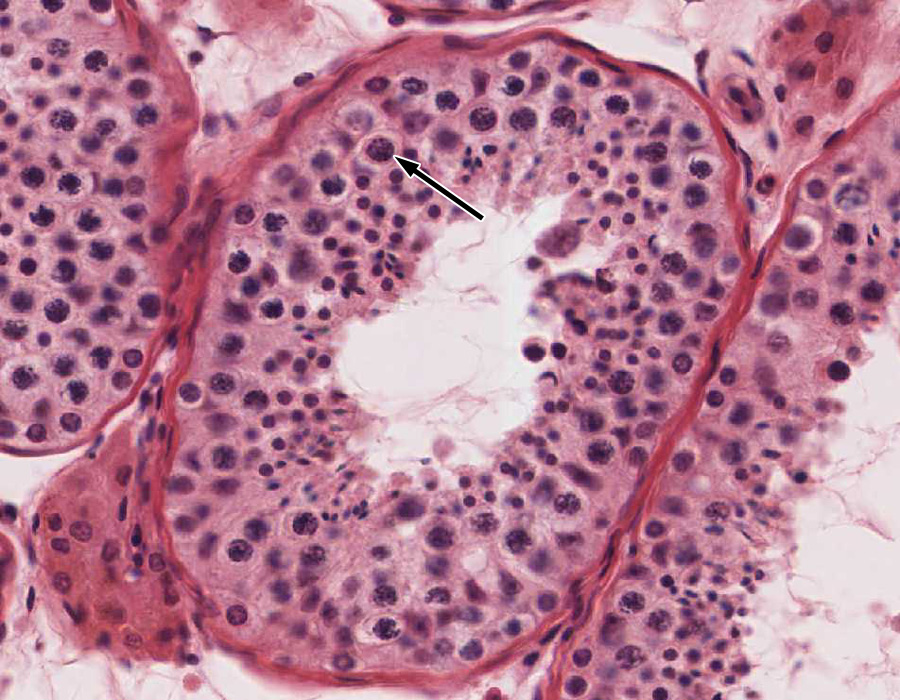
7. By convention, the ploidy (n) and DNA content (c) of a quiescent, diploid somatic cell is said to be 2n, 2c. What is the ploidy and DNA content of the cell indicated by the black arrow?
- 2n, 4c
- 1n, 2c
- 2n, 2c
- 1n, 2c
- 1n, 1c
Answer
Correct answer 1., 2n, 4c. The cell indicated is a PRIMARY SPERMATOCYTE that is clearly in the pachytene stage of meiosis I. At this stage, the cell has replicated its DNA, so it is diploid (2n) and has twice the normal amount of DNA (4c).
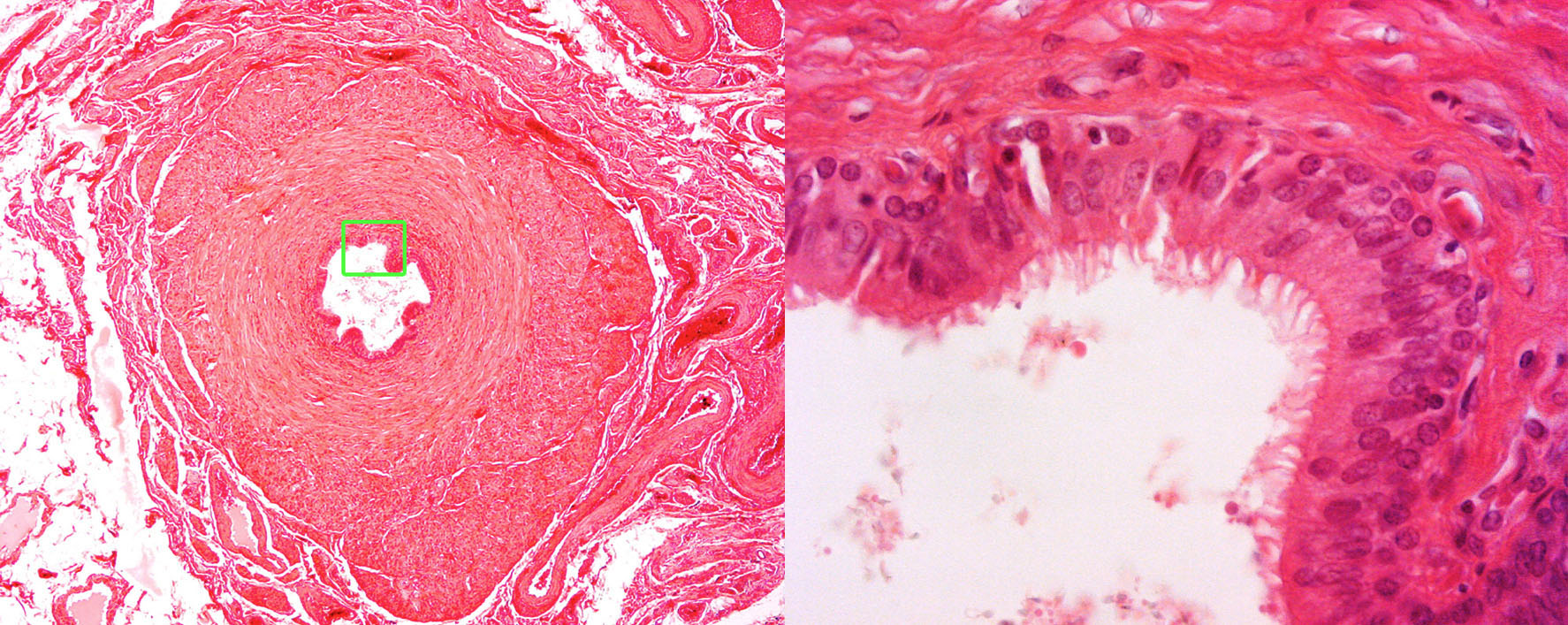
8. The asterisk (*) marks the lumen of which histological structure/organ?
- A ductus (vas) deferens
- An efferent duct
- The epididymis
- A penile urethra
- An uterine (or intramural) segment of the oviduct
- The cervical canal
Answer
Correct answer 1., a ductus (vas) deferens. Note the stereocilia in the high mag view. These may be distinguished from true cilia at the EM level by the ABSENCE of basal bodies.
9. Identify the region/tissue shown in the below micrograph.
- Penis, corpus cavernosum
- Penis, corpus spongiosum
- Early placenta
- Late (term) placenta
- Seminal vesicle
- Ductus (vas) deferens
Answer
Correct answer 2., the corpus spongiosum. Note the penile urethra, which is lined by a mixture of stratified non-keratinizing epithelium and transitional (or urinary) epithelium.