Bone Formation and Remodelling
- Be able to describe and recognize in microscope sections the process of intramembranous bone formation.
- Understand where osteogenic stem cells are located and how they are involved in bone formation.
- Recognize different bone cell types: osteoblasts, osteocytes, and osteoclasts. Know their role in the process of intramembranous bone formation.
- Have an understanding of bone remodeling over time (osteon formation) and long bones growth in length and width.
- Recognize mature and immature (mottled or woven) bone in light micrographs.
- Understand the process of endochondral bone formation and know how a cartilage model is broken down and replaced by bone (e.g., formation of a bony collar, chondrocyte death or transdifferentiation, etc.).
- Be able to recognize the different zones of an epiphyseal growth plate and describe the processes that take place in each zone (e.g., zones of resting cartilage, proliferation, hypertrophy, calcification, and ossification).
- Be able to describe how bone fracture repair resembles the process of endochondral bone formation.
There is no single perfect section in which to study bone and its formation. The process involves transitions, and the various stages are simply too many to be encompassed in any one section. Even the many slides available in this session may not have all the structures you need for study, so try to look as many different slides as you can. With the exception of slide #51 and #93, all the slides you study have been decalcified by the action of acid or a chelating agent, so you will be looking at the remaining organic matrix. Bone is difficult to cut in paraffin so there are distortions and differential shrinkages, common events that lead to an almost universal separation of the bone from the periosteum. If you look long enough, however, you'll find intact areas; these areas are the ones with which to start your study.
Slide 46-HE (embryonic face, H&E) View Virtual Slide
Slide 46-M (embryonic face, Masson trichrome) View Virtual Slide
Slide 46-M-N (new scan of slide 46M) View Virtual Slide
Slide 120 (head, 66mm embryo, H&E) View Virtual Slide
Slide 120-N (new scan of slide 120) View Virtual Slide
These sections of human faces exhibits all stages of intramembranous bone formation. They are sections of a fetal human face stained with either H&E or H & Masson. You should be able to find:
- deposition of osteoid, (difficult to see but you can find examples in slides #46-HE View Image and #120 View Image ).
- a shift in matrix color (darker) with mineral deposition,
- osteoblasts (active and inactive) and osteoclasts View Image ,
- osteocytes , and
- forming Haversian systems or osteons (evident in slide 46-HE View Image and slide 46-M View Image ). In order to find all the structures listed above, you will have to look at many different spicules or trabeculae of bone.
Slide 115-N (palate, H&E) View Virtual Slide
Slide 115-M (palate, Masson) View Virtual Slide (note: this slide is a bit dark)
Further stages of developing a compact bone from a spongy one are illustrated in this parasagittal section of the palate. Note the increased numbers of osteocytes, in some places forming one or two rings of an osteon. In the H&E section, the rapidly formed, immature bone (aka "woven" bone) View Image exhibits a greater affinity for hematoxylin and higher cell density compared to mature bone. An outer fibrous layer and loose inner layer of periosteum can be seen. Sharpey's fibers made primarily of type I collagen spanning the cellular layer of periosteum and inserting into the bone are well illustrated in the both the H&E View Image and Masson-stained View Image sections.
Slide 48 (leg, 154mm embryo, H&E) View Virtual Slide
Slide 48b (leg, 154mm embryo, Masson) View Virtual Slide
One slide is stained with H&E, while the other is stained with trichrome. Only long bones grow in length by proliferative activity at theepiphyseal plate and subsequent endochondral ossification. Appositional growth increases their circumference. New bone is laid down around the shaft of a long bone by a mechanism that is essentially the same as that of intramembranous ossification (many authors use this term to describe the process--which can confuse you!). In this cross section of the developing tibial and fibular shafts (two stains again) note particularly the osteoblastic activity, and the forming osteons at the outer edge of the shafts in the H&E View Image and trichrome sections View Image. With the Masson stain you may see collagen fibers View Image running from the fibrous periosteum to the bone --what are they? (hint: refer to slide 115 above) The purple area in the Masson stained section is calcified cartilage - see endochondral section that follows.
Slide 49 20x (humerus, H&E) View Virtual Slide
Slide 49 40x (humerus, H&E) View Virtual Slide
There are two different magnifications (20X and 40X) of the epiphysis of a human long bone (those of you with even locker numbers may have a canine specimen on slide 49 that is much better). We require you to recognize 5 zones: 1) resting or reserve (R); 2) proliferative (P); 3) hypertrophy (H); 4) calcification (D); and 5) ossification (O). These specimens do not permit an actual distinction between hypertrophic and calcification, but make sure you understand the sequence ! Note the persistence of the cartilage cores well into the marrow cavity. Please remember that the zone of hypertrophy is the weakest region of the epiphyseal growth plate. It is here that the process of cartilage calcification is starting and no bone has yet been deposited on its surface. Therefore, it is prone to breakage in children. Also find the secondary center of ossification View Image in slide 49 that is just starting to form in the head of the bone (there are blood vessels present in the cartilage, but it hasn't yet started to ossify); the primary center of ossification is in the shaft of the bone. Note that hyaline cartilage in the head of the bone, while avascular, certainly contains spaces for traversing large blood vessels indicative of bone formation. An example in which bone can actually be seen in the secondary ossification center may be found in slide 61 in the UCSF collection View Image.
Slide 108 (finger, H&E) View Virtual Slide
Slide 110 (finger, H&E) View Virtual Slide
Slide 47 (knee, sheep embryo, H&E) View Virtual Slide
These slides are useful for looking at other examples of endochondral ossification because you can see the entire forming bone and adjacent joint cavities. Look at the cartilage ends (epiphyses) and the forming bony shaft using the two phalange slides (Slides 108 and 110). The process can be seen more easily in slide 108 View Image than in slide 110 View Image . Also examine the periosteum and forming marrow cavity. Slide 47 View Image of a developing knee joint also illustrates endochondral bone formation quite well. The intense basophilia present in the zone of ossification is likely due to abundant glycosaminoglycans (GAGs) associated with proteins (e.g. ostenectin, osteocalcin, and ostepontin) involved with the early stages of matrix ossification.
Note: this section is repeated from the Cartilage/Mature Bone lab session. However, NOW you know what "interstitial lamellae" are and how they form, so be sure you can identify them.
Slide 50 (compact bone, decalicified, H&E) View Virtual Slide
Even though this section is distorted, you should be able to find osteons in various stages of development, lacunae, and canaliculi (to see canaliculi you will need to use your microscope and the glass slide from your collection --cut down the light by closing down the iris diaphragm to see them). Incremental deposition similar to that which would be present in inner and outer circumferential lamellae can be seen.
Ground sections:
Slide 51 (cross section) View Virtual Slide
Slide 93B (cross section) View Virtual Slide
Slide 93A (longitudinal section, thin) View Virtual Slide
Slide 51 (longitudinal section, 20x) View Virtual Slide
Slide 51L-EX (longitudinal section, 40x) View Virtual Slide
Slide 93C (longitudinal section) View Virtual Slide
There are both longitudinal and cross sections. First, study cross sections (slides 51 and 93B). In these sections, the trapped air bends the light giving a dark image; the mineral and matrix generally transmit the light. You should be able to identify osteons and their subdivisions (as in slide 50), interstitial lamellae, Haversian/central canals and nutrient canals (Volkmann). Note that the latter canals penetrate osteons without causing new lamellae to be laid down around them. Study the thinnest ground section (#93A) to identify lacunae and canaliculi. (in this figure the tissue is "unstained" but a red dye has been used to illustrate canals, lacunae and canaliculi). Now, look at the longitudinal sections (slides 51-20x, 51-40x, or 93C) of compact bone and try identifying the various structures mentioned above, especially Haversian/central and Volkmann's canals.
84 Intramembranous Bone Formation View Virtual EM Slide
This is sometimes called "direct" bone formation because it does not involve cartilage. Hence, chrondocytes would not be found in this section. The term "membrane" is used here because the periosteum around forming bone appears like a membrane. Make sure you know the structural and functional differences between an osteoblast and osteocyte. Observe (and remember) that the bone formation, which occurs from the periosteum of the diaphysis of long bones is identical to the process of intramembranous bone formation. In this unique micrograph, study the differentiation of osteoprogenitor cells to osteoblasts and subsequently to osteocytes. What is osteoid? (BO8) Note the formation of long cell processes as the osteoblast (lower right corner) prepares for the transformation into an osteocyte. Find the cell process, which is already located in a canaliculus.
90 Osteocyte View Virtual EM Slide
The calcium crystals of the bone matrix were removed in this preparation by a decalcification process. Note how coarse the collagenous fibrils are and the difficulty in visualizing the periodicity of the fibrils (probably due to the process of mineralization).
83 Cartilage Endochondrial Ossification (Zones of Chondrocyte Proliferation and Hypertrophy) View Virtual EM Slide
Study the transition that occurs in the chondrocytes as they change from very active to hypertrophied and dying. Why do the chondrocytes die?(BO9)
86 Bone Metaphyseal Plate Endochondrial Ossification (Zones of Hypertrophy and Calcification) View Virtual EM Slide
Study the changes that are associated with the removal of the cartilage and the deposition of a bone matrix.
91 Bone - Osteoclast View Virtual EM Slide
The osteoclast is a very large cell (multinucleated) that sits on the surface of bone matrix. Note the many lysosomes and phagocytic vacuoles. What is the functional significance of these structures?(BO10). Most osteoclasts are thought to arise by fusion of monocyte-macrophages
93 Haversian/Central canal View Virtual EM Slide
Note the "inactive" appearance of endosteal cells. The presence of a macrophage in the Haversian/central canal indicates the potential eroding function of the endosteal lining of the canal. Why are blood vessels so important in bone? (MatureBO2)
Click on a question to reveal the answer.
How does the diameter of the bone shaft increase with growth?
The bone shaft increases in diameter by appositional growth. New bone is deposited on the outer surface of the diaphysis by successive generations of osteoblasts arising from osteogenic cells of the periosteum. To compensate this growth and prevent bone from becoming too thick and heavy, older bone on the inner surface of the shaft is being resorbed by osteoclasts so as to widen the marrow cavity.
What is the functional significance of lysosomes and phagocytic vacuoles present in osteoclasts?
The degradation of mineralized bone matrix is considered to be due to focal decalcification and extracellular digestion by acid hydrolases and other enzymes contained in lysosomes.
Why are blood vessels important in bone?
Bone is a living tissue and, as such, needs a constant supply of nutrients. Without blood vessels, the bone would die.
What will fill the cavity of long bones when they are fully developed?
Bone marrow is found in the bone cavities of long bones and is involved in the production of blood cells. Marrow is also found in the cavities of flat bone.
Where is the endosteum?
Endosteum is the lining of the marrow surface. It is important to note that the absence of endosteum or periosteum on a bone signals that the bone is ready to be reabsorbed by osteoclasts. Bone cannot be bare. It is always covered by something or else it will be reabsorbed.
Can you see fibrous and cellular layers of the periosteum?
You should be able to see them. The fibrous layer of periosteum is made up of collagen fibers and fibroblasts. The cellular layer consists of osteoprogenitor cells, which can divide and produce osteoblasts. The endosteum is composed solely of a layer of osteoprogenitor cells.
What will happen to the cartilage cores that persists in bony spicules (trabeculae) in the marrow cavity?
Some cartilage cores will remain as such for some time in boney trabeculae. Eventually, most trabeculae become resorbed and replaced by lamellar bone. The cartilage cores in bigger and thicker trabeculae will be invaded by blood vessels, osteoblasts and osteogenic cells that lay down concentric lamellae of bone replacing cartilage cores.
What is the correlation between woven, spongy and compact bone and intramembranous and endochondrial bone formation?
There is very little correlation between these things. In terms of the three types of bone, the differences between spongy and compact bone will be discussed in the next question. Woven bone is rapidly formed, new bone and is a precursor to both of these types of bone. Intramembranous bone takes place in mesenchymal tissue and is the type of formation of most of the flat bones of the body (skull, mandible, etc.). It involves the direct formation of bone by osteoblasts and does not involve a cartilage precursor. Both compact and spongy bone can form in this way. Endochondrial bone formation begins with a cartilage precursor that proliferates, hypertrophies, and becomes imbedded in the core of bone. This method is most common in long bones of the body (like the shaft of the femur). An important point, here, is that cartilage does not become bone. Rather, bone is deposited on the surface of calcified cartilage. The type of bone formation does not correlate with the type of bone formed. The difference in the types of bone formation is the way in which the bone is initially formed, not in the end result.
What distinguishes between compact and spongy bone?
Though it is easy to differentiate between compact and spongy bone at a gross level, at the microscopic level the main difference is the presence or absence of osteons. Grossly, compact bone has a dense appearance and is found, for example, on the outer surfaces of the long bones of the body. As the name implies, spongy bone is shaped like a sponge. The spaces within the sponge-shaped framework are filled with bone marrow. Compact bone, microscopically, is made of numerous osteons, whereas spongy bone is composed of sheets of lamellar bone and does not contain osteons.
What is osteoid?
Osteoid is the organic matrix of bone, not yet mineralized, that is laid down by osteoblasts (which also facilitate its mineralization).
Why do chondrocytes die after they hypertrophy in the epiphyseal plate of the metaphysis?
Because of calcification, the chondrocytes lose all sources of nutrients, etc. and die.
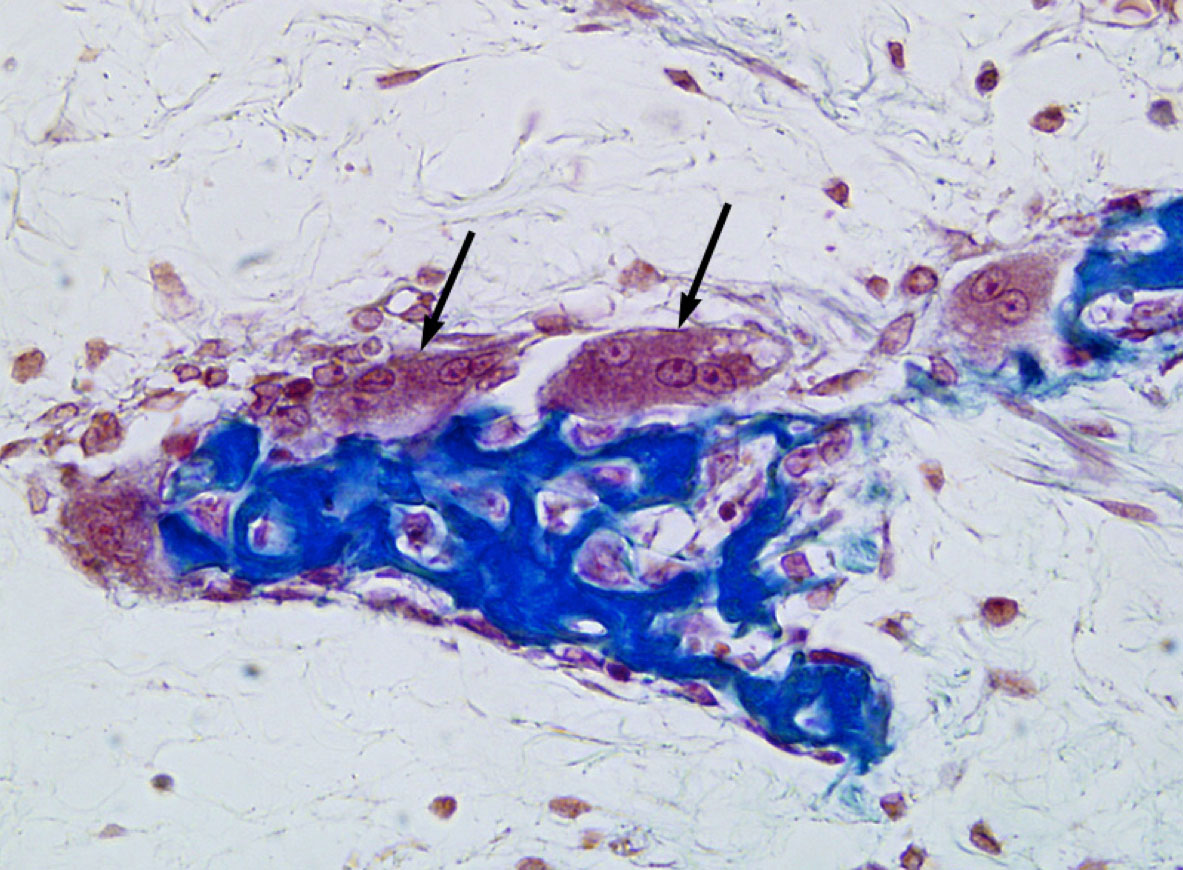
1. Which of the following statements regarding the cells indicated by the black arrows is INCORRECT?
- They are derived from hematopoietic progenitor cells.
- They secrete collagenase.
- They are involved in remodeling ALL bones, whether formed via endochondral OR intramembranous ossification.
- Excess activation of these cells may result in hypocalcemia (low blood calcium levels).
- NONE of the above (i.e. ALL of the above statements are CORRECT).
Answer
Correct answer 4. as its statement is incorrect. The activation of osteoclasts results in higher blood calcium levels. Low blood calcium levels will trigger the release of parathyroid hormone (PTH), which will induce the formation of new osteoclasts.
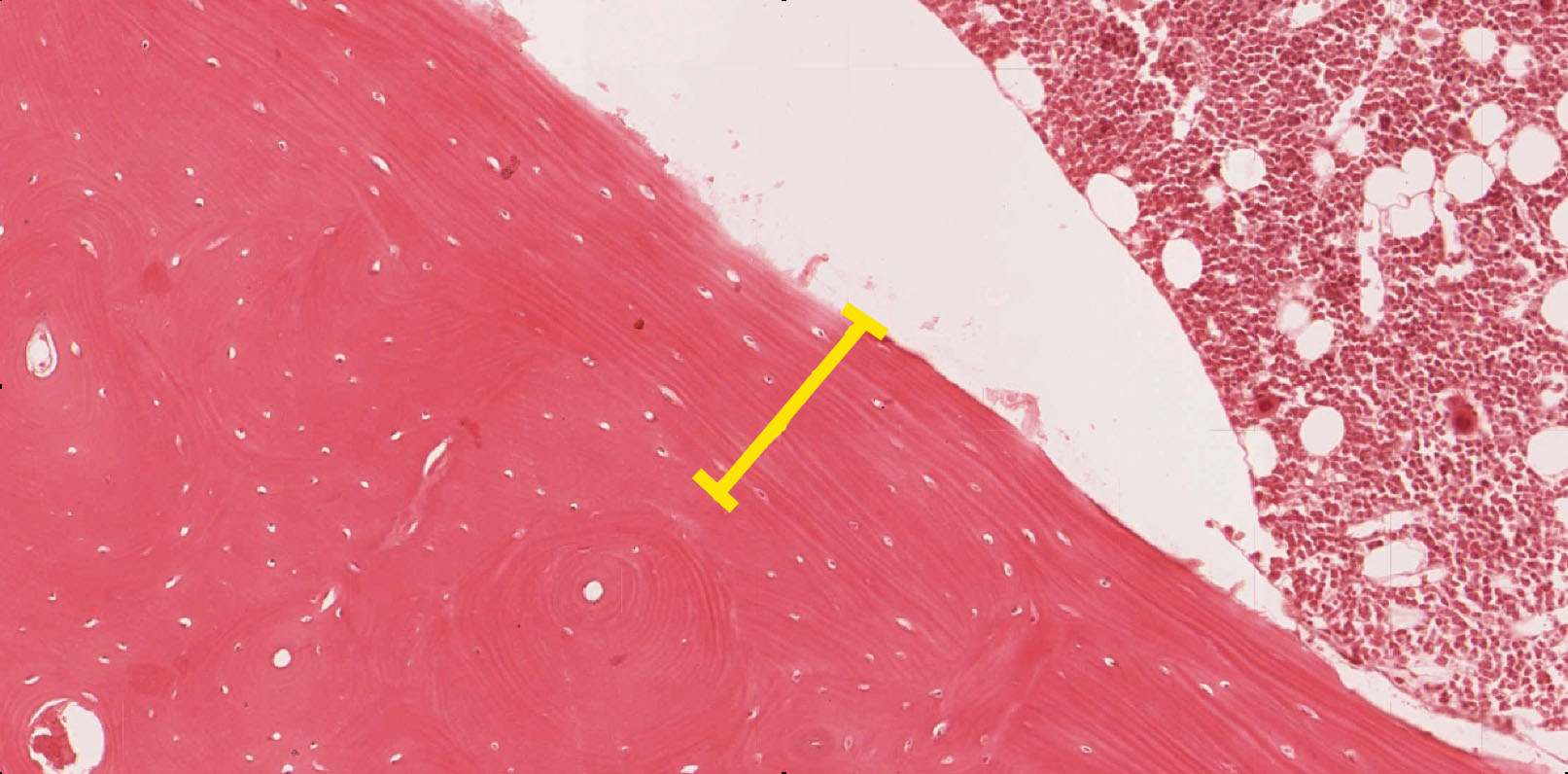
2. What histological structure does the yellow bracket indicate?
- An interstitial lamella
- An inner circumferential lamella
- An outer circumferential lamella
- The periosteum
- The endosteum
Answer
Correct answer 2. The inner circumferential lamella is labeled. Note the location of the bone marrow.
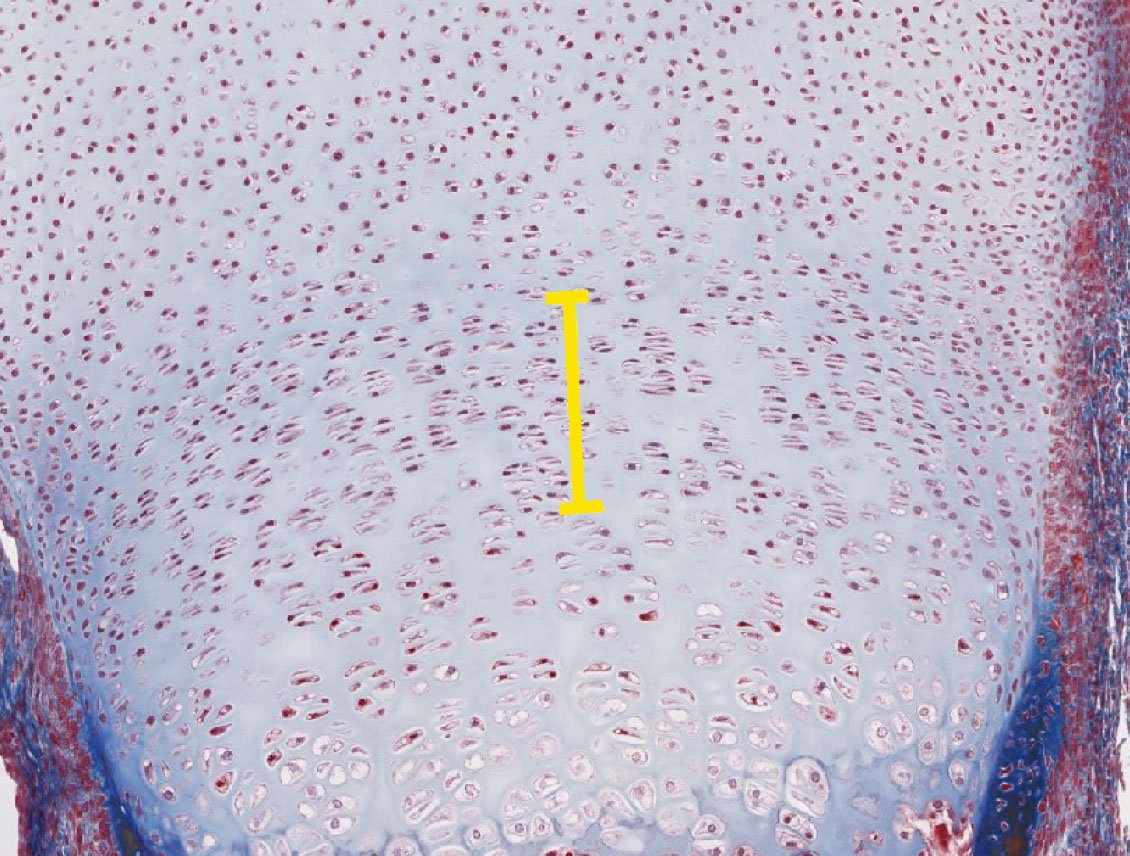
3. Select the answer that best describes the area indicated by the yellow bracket.
- It contains proliferating chondrocytes.
- It contains type II collagen fibers in its matrix.
- It is NOT present in adult bone (bone that is no longer growing in length)
- ALL of the above statements (1 to 3) are true
- None of the above statements are true
Answer
Correct answer 4. All of the first three statements are true as the image depicts an epiphyseal growth plate with the zone of proliferation marked by the yellow bracket.
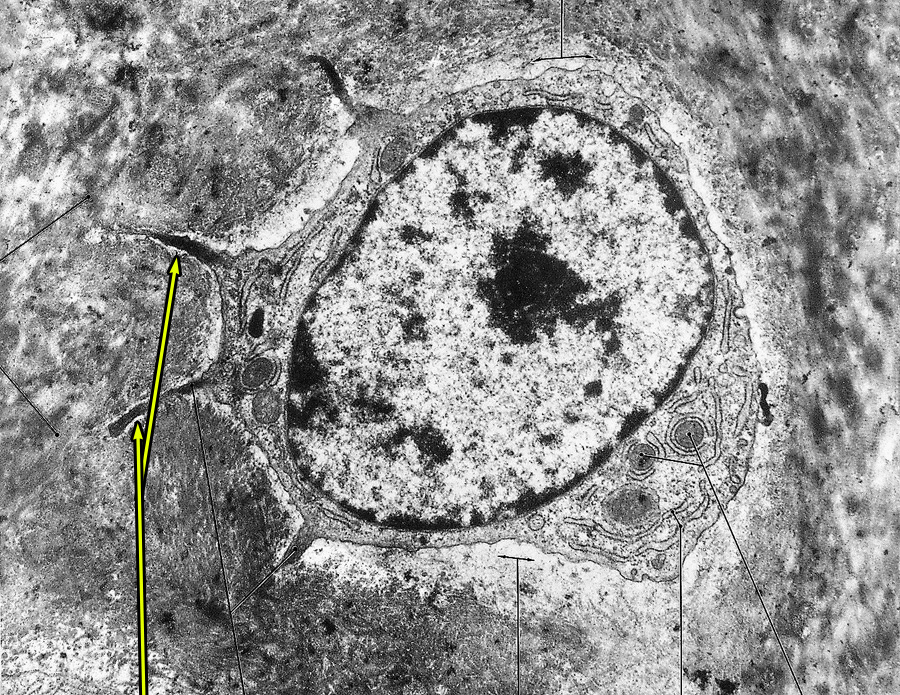
4. Identify the indented regions indicated by the yellow arrows.
- Lacunae
- Canaliculi
- Haversian canals
- Volkmann's canals
- Howship's lacunae
Answer
Correct answer 2. The yellow arrows indicate canaliculi that extend from an osteocyte in a lacuna.
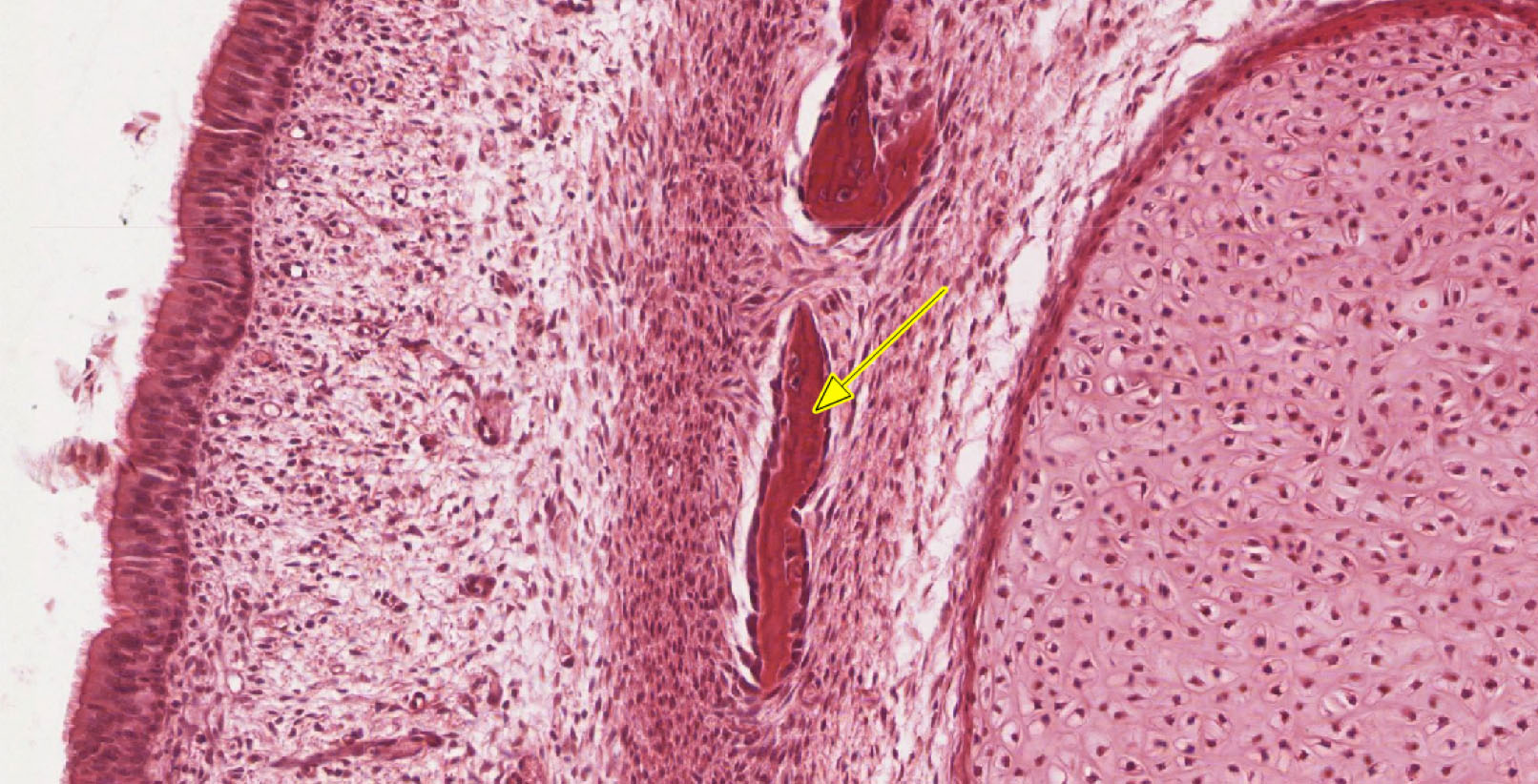
5. Which statement(s) is/are true about the structure indicated by the yellow arrow.
- It arose via intramembranous ossification.
- It arose via endochondral ossification.
- It is comprised primarily of calcified cartilage.
- It is undergoing extensive remodeling as evidenced by numerous osteoclasts on its surface.
- It is in a secondary center of ossification.
Answer
Correct answer 1. The bone spicule arose by intramembranous ossification.