1. Be able to recognize and classify different epithelial tissues.
2. Be able to correlate different types of epithelia with their locations and functions.
3. Know the structure and function of different cell-cell and cell-substrate junctions.
4. Know the structural aspects of apical specializations (microvilli, stereocilia, and motile and sensory cilia) and their functions.
5. Be able to recognize various cell organelles and cell junctions in EM micrographs and to identify striated or brush borders and cilia by light microscopy and EM.
In epithelia, cells are organized in sheets, either a single layer thick (simple epithelia) or made up of multiple layers (stratified epithelia). Be able to identify the classes of epithelia underlined in the text below, and give some thought to why these different classes of epithelia have such different morphologies. The glass slide sets occasionally contain different stains or even different slides of the same tissue in place of the slide that you have in your set. When these differences occur, the lab guide will usually refer to a particular slides as being in either even or odd-numbered slide collections. Please try to look at the alternates by borrowing from your lab mates. Certain stains are much more instructive than others and different (alternate) tissues often help to explain functional changes.
A. Simple columnar epithelium
Slide 29 (small intestine) View Virtual Slide
Slide 176 40x (colon, H&E) View Virtual Slide
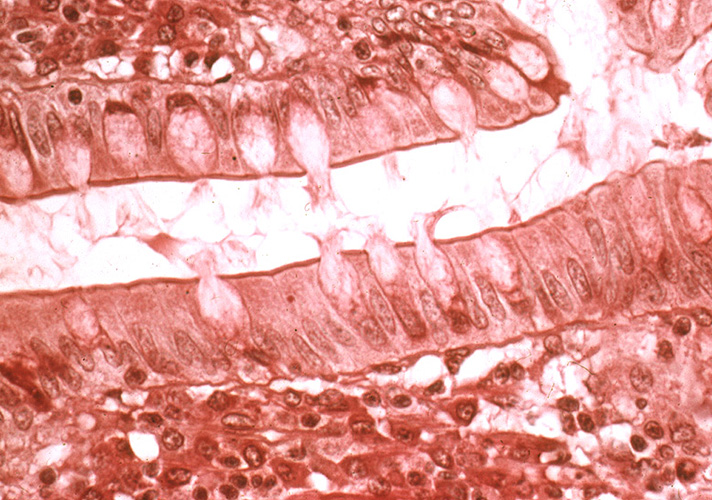
Remember that epithelia line or cover surfaces. In slide 29 and slide 176, this type of epithelium lines the luminal (mucosal) surface of the small and large intestines, respectively. Refer to the diagram at the end of this chapter for the tissue orientation and consult the atlas for the cell types that make up the epithelium. First, examine slide 29 at low power and note finger-like projections of intestinal villi. Also, note that, in some areas, these villi are transversely sectioned and appear instead as circular profiles. The villi are lined by a simple epithelium, and, therefore, you should ideally see a single row of dark nuclei toward the base of the cells (you may see more if the epithelium is cut tangentially). Also, it is a columnar epithelium, so the cells should be taller than they are wide. Look around on the slide until you find a region of epithelium having this appearance. Note the presence of goblet cells, which look like balloons suspended in the epithelium. These cells secrete mucus; the clear "balloon" in the apical region of each goblet cell is where the stored mucus is located (mucus does not react with H&E stain). Look at the columnar epithelium in slide 176 and note that it contains a very large population of goblet cells relative to that found in slide 29. In the colon, villi are absent and, instead, a simple columnar epithelium forms the intestinal "glands," which are invaginations made up of mostly goblet cells. Identify the microvillous border at the apex of the epithelial layer at 40x magnification in slide 29. This region appears as a darker staining line at the top of the cells. In a very good section, it may appear striped, or "striated", because it is made up of finger-like projections called microvilli (seen at the electron microscopic level in EM #213).
B. Simple cuboidal epithelium
Slide 9N-1 kidney, H&E View Virtual Slide
Slide 210 kidney, H&E View Virtual Slide
These slides show simple cuboidal epithelium, lining tubules in the kidney. The tubules are cut in all different orientations; look for a region toward the middle of the slide where the tubules are cut more or less in longitudinal section in slide 9N-1 View Image or slide 210 View Image and appear as parallel wavy rows (at 4x magnification). Look for a favorable area where you can see a space (the tubule lumen) lined on either side with simple cuboidal epithelium. Note also that there is very little other tissue between tubules, so that you often see two rows of cuboidal epithelia from adjacent tubules back to back. In other parts of the section, look for tubules in cross-section in slide 9N-1 View Image or slide 210 View Image where the lumen will be surrounded by a circle of cells.
C. Simple squamous epithelium
Slide 30 (mesentery, H&E) View Virtual Slide
Slide 29 (small intestine) View Virtual Slide
Simple squamous epithelial cells are flattened, i.e., wider than they are tall. A simple squamous epithelium, called "endothelium," lines blood vessels, lymphatic vessels, and the chambers of the heart. When sections through endothelial cells are viewed with the light microscope, the cytoplasm cannot be seen, because the flattened cell is so thin. Thus, endothelium is generally identified on the basis of the structure and position of nuclei alone; that is, the nuclei are also often flattened and elongated, and are found lining the lumen of the vessel. Observe the endothelial lining of blood and lymph vessels in the mesentery in slide 30 View Image. Sometimes the blood vessels contain red blood cells and can be identified that way. Otherwise, look for tubular or circular profiles at low power and examine the endothelial lining of these vessels at high power. Note that the endothelium may be damaged during processing such that it separates from the vessel wall or it may slough off entirely and not be visible at all. In areas where you can find an endothelium, note that the nuclei do not always look flattened in vessels that have contracted. Another excellent place to look for endothelial cells is in the many small vessels in the wall of the intestine shown in slide 29 --look for the vessels in the submucosal layer (the lightest staining area in the wall of the intestine) View Image.
Going back to slide 30, move to the periphery of the tissue section and observe a simple squamous epithelium (flattened cells) covering the surface of the mesentery View Image. This epithelium --also called mesothelium-- and the irregular connective tissue immediately underneath together make up the peritoneum (a term that you will encounter in your anatomy studies) that lines body cavities and most of the viscera contained therein. Specifically, the portion of the peritoneum that is applied against the walls of the cavities is known as "parietal peritoneum" whereas the portion covering the organs (and their associated mesenteries) is the "visceral peritoneum."
A. Stratified squamous epithelium
This type of epithelium covers surfaces that are subjected to abrasion. The epithelium is constantly replacing itself by division of the basal layer of cells. These cells change morphology as they move toward the surface and are ultimately sloughed off. They are called "stratified" because there are multiple cell layers, and "squamous" because the outermost layer of cells is flattened. There are two subclasses:
1. Stratified squamous nonkeratinizing epithelium
Slide 153 (esophagus, H&E) View Virtual Slide
Slide 126 (trachea, esophagus) View Virtual Slide [see orientation]
Slide 250 (vagina, H&E) View Virtual Slide
This type of epithelium covers some internal surfaces that are kept moist by mucus or other fluids. Thus, these epithelia do not need to keratinize to avoid desiccation. The lubrication provided by mucus helps to protect against abrasion. Study this type of epithelium in the esophagus (slide 153) and vagina (slide 250). Again, cell morphology changes from base to apex of the epithelium, the outermost being "squamous" in appearance whereas the basal cells appear more cuboidal or low-columnar. The orientation of the tissue can be confusing because of connective tissue projections that push up into the epithelium. Unlike keratinizing epithelium, nuclei are still present in most surface cells (although they are often difficult to see in sectioned tissue.)
2. Stratified squamous keratinizing epithelium
Slide 106 (plantar skin, H&E) View Virtual Slide
Slide 112 (plantar skin, H&E View Virtual Slide
This epithelium is found at the surface of the skin and is known as the epidermis. As protection against desiccation, it undergoes a process known as cornification or keratinization. As cells move toward the surface, they differentiate and eventually die, leaving an outermost layer of dead cells filled with keratin View Image. The absence of nuclei in this layer shows that it is devoid of live cells. In some slides, the keratinized region is gray, but occasionally it has been penetrated in places by red stain. Note the differences in morphology of the cells as they move toward the surface. You will learn the names of these layers when we study the skin. In the lower strata, look for the layer of spinous cells (the spines look like little lines between cells, and can be difficult to see) View Image; the spines are sites where desmosomes attach the cells to one another.
B. Pseudostratified epithelium
Slide 40 (trachea, H&E) View Virtual Slide
Slide 126 (trachea, esophagus) View Virtual Slide [see orientation]
"Pseudostratified" is a term applied to epithelia that appear to be stratified (i.e., have nuclei at various levels), but in which all component cells reach the base of the epithelium and are attached to the underlying basement membrane. The basement membrane looks like a pink line at the base of the epithelium, which is rather easily seen in places on this slide. The basement membrane is not always this thick in other epithelia (Note that "basal lamina" is a term that refers to an ultrastructural feature while "basement membrane" refers to a light microscopic feature. Ultrastructure refers to structures seen at the electron microscope level. Only some of these cells reach the free surface of the epithelium, where it is generally ciliated and contains goblet cells. Since this type of epithelium lines the respiratory tract, it is referred to as the "respiratory epithelium". The cilia appear as hairlike projections at the cell apex.
What substructures form the core of each cilium?
Answer
The core of a cilium is made up of an axoneme, consisting of a 9+2 array of microtubules.
C. Transitional epithelium
Slide 211 (nondistended ureter, human, H&E) View Virtual Slide
Slide 19-1, "odd" (distended ureter, rat, H&E) View Virtual Slide
Slide 19-2, "even" (non-distended ureter, rat, H&E) View Virtual Slide
Duke University Slide 98, (non-distended bladder, H&E) View Virtual Slide (virtual slide courtesy of Duke University)
Transitional epithelium is confined to the urinary tract and is adapted for extensibility and water impermeability, as when the bladder fills with urine. We will compare the epithelium lining the lumen of a distended (slide 19-2) and a non-distended ureter (slide 19-1). In the non-distended ureter, note the shape of the large surface cells, which are frequently dome-shaped and may bulge out into the lumen. Now, compare with the distended ureter (this tissue was artificially over-distended to make a point about the capacity of this epithelium). The surface cells have been stretched thin, as have the other layers, and there actually appear to be fewer layers, as the cells can slide past one another to a certain degree.
While understanding the light microscopic structure of tissues and organs is important for interpreting pathological change, much of the really interesting biological side of medicine now involves understanding cell structure in more detail. Therefore, we feel you should be comfortable with interpreting electron micrographs by the time you complete your histology course, as they are becoming more important in diagnosis and many of the micrographs in your professional literature will be of this sort. We assume that you already have a general knowledge of cell ultrastructure and can recognize the nucleus, mitochondria, cell membranes, endoplasmic reticulum and ribosomes. The Wheater's Atlas contains an excellent review of cell ultrastructure, as does the Pawlina text. Please review these structures in these sources and the electron micrographs listed below and in the other chapters.
156 Cilia - Cross-sectioned in human trachea View Virtual EM Slide
Cross sections of cilia. The typical 9+2 arrangement of the microtubules is especially evident. The basal bodies are centrioles and have 9 triplets of microtubules with no central pair.
213 Small intestine - microvilli View Virtual EM Slide
Study the typical appearance of microvilli on the apical surface of this cell forming part of the striated or brush border in small intestine.
16 Epithelium - Desmosome and Intermediate Filaments View Virtual EM Slide
A desmosome can be seen in the upper right corner of this transmission electron micrograph. The cytoplasm is full of intermediate filaments (tonofilaments), some of which are attached to the desmosomal plaque.
120 Left Atrioventrical Valve - Bicuspid or mitral valve Simple Squamous Epithelium View Virtual EM Slide
The endocardium, the simple squamous epithelial lining of the heart, can be seen at the top of this section. Under it, you can see connective tissue, which we will study next time. Note how thin the epithelium is.
170 Kidney - Cortex, proximal tuble Brush Border View Virtual EM Slide
This EM micrograph depicts the typical appearance of microvilli on the apical surface of two types of cells with a striated or brush border. Shown is the epithelial lining cell of a proximal tubule in the kidney.
65 Epidermis Stratified Squamous Keratinizing Epithelium. VIew VIrtual EM Slide
You can appreciate that this epithelium (skin) is stratified (has multiple layers of cells) and that the layers near the surface (at the top of the micrograph) have keratinized (lost their nuclei and become a layer of keratin). The spiny appearance of cells deeper in the epithelium can also often be seen in the light microscope. They are points of cell-cell attachment, made more obvious by shrinkage during preparation. What junctions are found here?
190 Esophagus - Stratified Squamous non-keratinized epithelium View Virtual EM Slide
Compare this micrograph to EM#65. This is the lining of the esophagus, where it is no longer necessary to have an outer keratinized layer to protect against desiccation, as it was for skin. Thus, the outermost layer is still cellular and contains a nucleus. Note again the spiny appearance of the cells, due to the desmosomal attachments.
153 Trachea - ciliated pseudostratified epithelium Respiratory View Virtual EM Slide
Compare the morphology of the goblet cells with that of the other cells of the epithelium. Note that most of them are filled with secretory product (mucus) and that they do not have cilia. The line indicates the plane of section on EM#154.
154 Trachea - Respiratory Epithelium Respiratory Epithelium (tangential section) View Virtual EM Slide
The yellow colored area indicates the outline of one cell (see previous wall chart #153 for plane of section). Note the tops of the goblet cells protruding between the cilia. What are the differences among cilia, microvilli, stereocilia and kinocilia (which you will come across later)?
183 Urinary Bladder – Section of Wall Transitional Epithelium View Virtual EM Slide
Transitional Epithelium. This micrograph displays the transitional epithelial lining of the bladder. The wall of the urinary bladder contains 3 layers of somewhat irregularly arranged smooth muscle.
Click on a question to reveal the answer.
What structures form the core of each cilium?
The core of cilium is made up of an axoneme, consisting of a 9 +2 array of microtubules
What junctions are found in the spinous layer of stratified squamous keratinizing epithelium?
The junctions found in the spinous layer are called desmosomes. The spinous layer of stratified squamous epithelium got its name because the desmosomes linking adjacent cells gives them a "spiny" appearance.
1. Identify the type of epithelium in this image. In which organ/organ system would expect to find this type of epithelium?
View Image
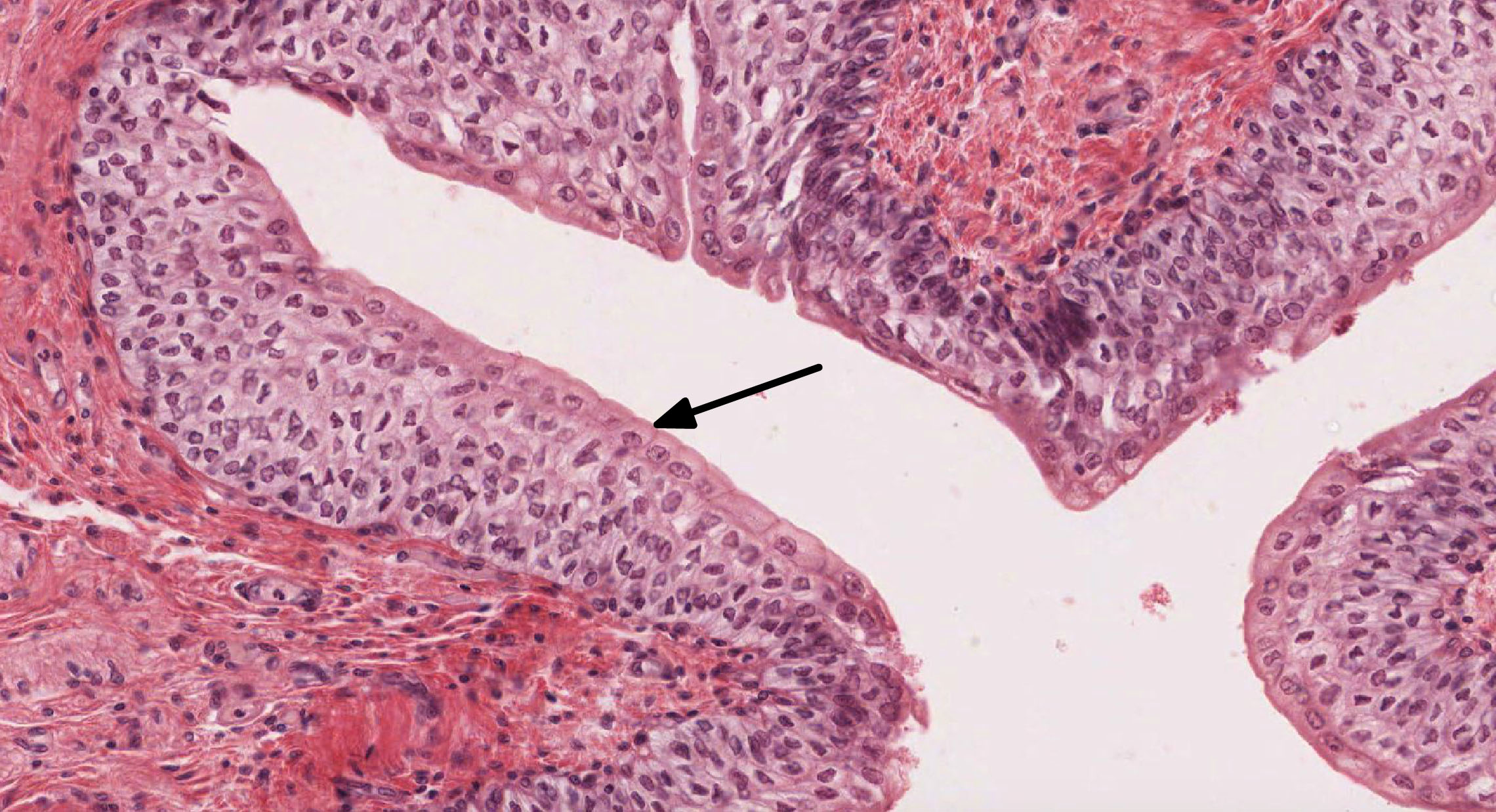
- The integumentary system
- The mucosa of the esophagus
- The respiratory tract
- The urinary tract
- The mesentery
Answer
Correct answer 4. The urinary tract - epithelium shown is transitional epithelium (note the DOME-shaped cells), which lines the urinary tract. (skin would be lined by stratified squamous keratinizing epithelium
2. Identify the type of epithelium that is depicted in this image.
- Simple cuboidal
- Simple columnar
- Stratified columnar
- Pseudostratified columnar (respiratory)
- Transitional
Answer
Correct answer 2. Simple columnar - the epithelium is simple columnar (with microvilli)
3. Which of the following statements regarding microvilli is FALSE?
- They contain a core of keratin intermediate filaments.
- They are anchored to the cell by a terminal web of intermediate and actin filaments.
- They are immotile (they do not move on their own).
- They facilitate absorption
- They are generally considered to be localized on the apical surface of epithelial cells.
Answer
Correct answer 1. They contain a core of keratin intermediate filaments. - The core of microvilli consists of ACTIN filaments
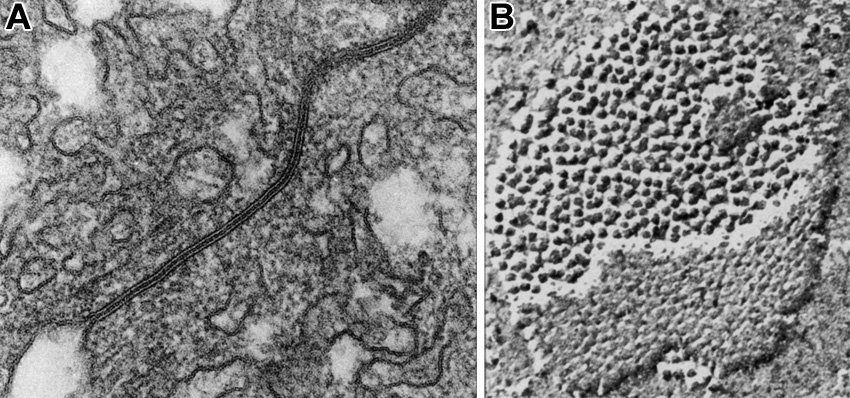
4. A type of intercellular junction as viewed by routine transmission electron microscopy in panel A and in a freeze-fracture preparation in panel B. Which statement about this type of junction is correct?
- It extends as a zone around the apical perimeter of adjacent cells.
- It posseses dense plaques that are anchored to intermediate filaments.
- It allows for the passage of ions from one cell to another.
- It requires calcium to bind adjacent cells.
- It mediates adhesion of cells to an underlying basal lamina.
Answer
Correct answer 3. It allows for the passage of ions (and other small molecules) from one cell to another. The junction shown is a field of GAP JUNCTIONs.