- Be able to describe the layers in the wall of the digestive tract (mucosa, submucosa, muscularis externa, and adventitia/serosa), and explain how they differ in the small and large intestinal segments.
- Know the three major strategies to increase the inner surface of the small intestine (plica circularis, villi, and microvilli with glycocalyx).
- Understand the structural arrangement of intestinal villi and glands.
- Know the different cell types found in the epithelium of the small and large intestine and be able to identify the most common cell types in light and EM micrographs. Know how epithelial turnover happens in the small intestine.
- Be able to identify and know the general functions and structural differences of the following regions of the lower GI tract: Duodenum, jejunum/ileum, colon, appendix, and rectum/anal canal.
To help you keep track of changes in the various layers, you can fill in this spreadsheet as you work through today's and next week's labs.
The histology of the wall of the small intestine differs somewhat in the duodenum, jejunum, and ileum, but the changes occur gradually from one end of the intestine to the other.
1. Duodenum
Slide 162 40x (pyloro-duodenal junct, H&E) View Virtual Slide
Slide 161 40x (pylorus, duodenum, pancreas, H&E) View Virtual Slide
Look at slide 162 first. Locate the duodenal portion in this slide and notice the presence of submucosal mucous glands (Brunner's glands). Observe that the ducts of these glands (and, occasionally, some acini) penetrate the muscularis mucosae and open into a crypt of Lieberkühn. After viewing slide 162, move to slide 161 and try to find the duodenal region in this tissue section.
2. Jejunum and ileum
Slide 29 40x (jejunum, monkey, H&E) View Virtual Slide
Slide 168 40x (ileum, H&E) View Virtual Slide
Slide 169 40x (jejunum, H&E) View Virtual Slide
Slide 170 40x (ileum, H&E) View Virtual Slide
Slide 165 40x (ileum, Alcian blue PAS stain) View Virtual Slide
Slide 171 20x (jejunum, vascular inj) View Virtual Slide
Slide UCSF 246 40x (jejunum, human, H&E stain) View Virtual Slide
Slide UCSF 247 40x (jejunum, human, H&E and silver stain) View Virtual Slide
View these sections with the low power objective and identify the mucosa, submucosa and the muscularis externa. Note that the mucosa consists of three sub-layers:
- epithelium
- lamina propria (or lamina propria mucosa –"propria" means "belonging to"
- muscularis mucosae (or lamina muscularis mucosae –"mucosae" here is not plural, but genitive, so this literally means "muscular layer of the mucosa")
The mucosa, which is clearly demarcated from the submucosa by the prominent muscularis mucosae layer, frequently shows heavy lymphocytic infiltration in the lamina propria.
The appearance of the submucosa layer is a bit variable, but, in general, it's best considered as irregular connective tissue: in slide 29 the submucosa appears more "loose" whereas in slides 168 and 170 it is more dense, and, in slide 169, here the submucosa is edematous and exhibits unusually dilated blood vessels. You can see the intestinal villi and intestinal glands (crypts of Lieberkühn). Examine the villi at a higher magnification and note that the lining epithelium consists of simple columnar cells (aka enterocytes) with a brush border and interspersed goblet cells, particularly well-demonstrated in slide 168. You can observe the distribution of goblet cells in the intestinal epithelium stained with PAS (slide 165).
The epithelium lining the villi continues into the intestinal glands. Examine several of these glands in slide 169 and note that goblet cells and enterocytes similar to those lining the villi, cover the upper portions of the gland. Also, notice that there are many mitotic figures View Image . The cells which line the lower portions of the crypts are less well differentiated. You may be able to see the enteroendocrine cells View Image in this region. These are the cells with spherical nuclei and clear cytoplasm --the secretory granules of these cells are not always stained very well, but, if they are, you should note that the granules are oriented basally.
Slides 246 View Virtual Slide and 247 View Virtual Slide from the UCSF collection have some excellent examples of enteroendocrine cells View Image. Again, the enteroendocrine cells have a clear cytoplasm and, if visible, basally-oriented granules. Slide 247 in particular has been stained with ammonium silver nitrate to demonstrate so-called "argentaffin" cells View Image (which, incidentally, are now known to be "S" or serotonin-secreting enteroendocrine cells --the serotonin in these cells reacts with the silver causing a black precipitate to form). Note that there are about 20 different types of enteroendocrine cell, and you are NOT expected to be able to identify a specific type of enteroendocrine cell (e.g. the "S" cells described above), but you should know the general histological characteristics and functions of enteroendocrine cells as a whole.
Paneth cells View Image occupy the base of the intestinal cypts/crypts of Lieberkühn. They are not well preserved in slide 169, somewhat better in slide 168, and quite good in slides 29 and 170. These cells are pyramidal shaped with round nuclei located near their base. They contain brightly eosinophilic (almost orange) secretory granules in the apical cytoplasm. In slide 168, the secretory granules in the Paneth cells stain a refractory brown or green.
Just under the mucosal epithelium is the lamina propria (or lamina propria mucosa), which consists of loose connective tissuethat fills the spaces between the intestinal glands and forms the cores of the intestinal villi. Within the core of each villus is a central lacteal, capillaries, and delicate wisps of smooth muscle that extend from the muscularis mucosae below. However, in some regions, the lamina propria may be so packed with a heavy infiltration of lymphoid cells that these finer structures may not be visible. You may hear the term "Peyer's patches" used to describe such regions in the GI tract. However, technically, Peyer's patches are found ONLY in the ileum and they are big enough to be visible with the naked eye.
The muscularis mucosae (or laminae muscularis mucosae) consists of smooth muscle fibers. Observe that strands of smooth muscle fibers from the muscularis mucosae extend into the cores of the intestinal villi along the central axis. Contractions of this muscle layer are controlled by ganglion cells and nerve fibers of the submucosal (Meissner's) plexus View Image located in the submucosa. The muscularis externa consists of two layers of smooth muscle: inner circular and outer longitudinal. Observe the ganglion cells and nerve fibers of the myenteric (Auerbach's) plexus View Image located between the two muscle layers.
The mucosa of the large intestine does not have folds comparable to the plicae circularis, except in the rectum. Also, the intestinal villi are absent beyond the ileocecal valve.
1. Colon
Slide 176 40x (colon, H&E) View Virtual Slide
The mucosa of the colon is lined by a simple columnar epithelium with a thin brush border and numerous goblet cells. Note that there areno plicae or villi. The crypts of Lieberkühn are straight and unbranched and lined largely with goblet cells. In many regions the mucus is partially preserved and stains with hematoxylin. At the base of the crypts, undifferentiated cells and endocrine cells are present; however, Paneth cells are not usually present. The appearance of the lamina propria is essentially the same as in the small intestine: Leukocytes are abundant and the isolated lymphoid nodules present in this tissue extend into the submucosal layer (survey the left lower area of slide 176). The muscularis mucosae is a bit more prominent compared to the small intestine, and consists of distinct inner circular and outer longitudinal layers. The submucosa of this specimen is particularly well fixed such that you may better appreciate the mixture of irregular connective and adipose tissue, numerous blood vessels, and several excellent examples of ganglion cells and nerves of the submucosal plexus. The muscularis externa of the large intestine is different from that of the small intestine in that the outer longitudinal layer of smooth muscle varies in thickness and forms three thick longitudinal bands, the taeniae coli (taenia = worm). This section happened to be cut such that a piece of one of these longitudinal bands may be seen.
2. Appendix
Slide 175 40x (appendix, H&E) View Virtual Slide
Study this slide and note the following characteristics.
- The mucosa resembles that of the colon, but...
- The muscularis externa resembles that of the small intestine in that it has an inner smooth muscle layer and a COMPLETE outer smooth muscle layer (i.e. the outer muscle layer is NOT bundled into taenia coli)
- Lymphoid nodules frequently accumulate in the submucosa, disrupt the muscularis mucosae and extend into the mucosa, almost approaching the luminal surface.
3. Recto-anal Junction
Slide 177 40x (recto-anal junct, monkey, H&E) View Virtual Slide
Slide 177-2 20x (recto-anal junct, human, trichrome) View Virtual Slide
Slide 177-3 20x (recto-anal junct, human, H&E) View Virtual Slide
Look at these slides (especially slide 177-3) at low magnification first to locate the recto-anal junction. Here you will observe a narrow zone of transition from the simple columnar epithelium of the intestine to the keratinized stratified squamous epithelium of skin. Within the transition zone, you may find stratified columnar (or sometimes cuboidal) epithelium followed by nonkeratinized stratified squamous epithelium. While looking, move the image from the colon toward the direction of the recto-anal junction. Observe that the crypts become shorter and shorter, eventually disappearing near the junction. Also observe that the muscularis mucosae becomes tattered and disappears, allowing the lamina propria merge with the underlying submucosa in this area. Note the presence of a large number of submucosal veins View Image. When these veins become dilated and varicose, they cause the mucosa to bulge and create the condition commonly known as hemorrhoids. Examine the skin lining the anal region and observe sebaceous and sweat glands, hair follicles, etc., particularly evident in slide 177-2 View Image. Also, note the massive amount of smooth and skeletal muscle that form the internal View Image and external anal sphincters View Image, respectively. The primate specimen (slide 177) shows these muscles quite well.
207 Small intestine (Muscularis Externa) View Virtual EM Slide
Study the orientation of the smooth muscle cells in the intestinal muscularis externa. The micrograph will help you understand the pattern, which arises from the inner circular layer and outer longitudinal layer of smooth muscle cells. Without the knowledge in which direction the intestinal epithelium is located, it is not possible to discriminate between the two sublayers of the muscularis externa.
208 Small Intestine - Tip of Villus View Virtual EM Slide
The villus is covered by a simple columnar epithelium. Note that cells are sloughing off at the tip of the villus. Find some goblet cells, which represent one resident cell type of the intestinal epithelium. The small lymphocyte is transient and is not a permanent component of the epithelium. Find the “striated border” and realize that you can’t resolve individual microvilli at this magnification. Study the composition of the connective tissue core of the villus.
213 Small intestine - microvilli View Virtual EM Slide
Study the typical appearance of microvilli on the apical surface of this cell forming part of the striated or brush border in small intestine.
211 Small intestine - Base of villus from rat jejunum (Simple Columnar Epithelium) View Virtual EM Slide
You can see that this type of epithelium, which is lining the lumen of the jejunum of the small intestine, is a simple epithelium. It is only one cell layer thick and columnar, as the cells are rather tall. Note the basal lamina at the base of the epithelium. In some places you can see the apical area where junctions are located. Most of these cells also have short apical microvilli.
214 Small Intestine - Crypts of Lieberkühn in Jejunum View Virtual EM Slide
In this simple tubular gland, Paneth cells are found near the end, whereas mucous cells and undifferentiated cells take up the major portion of the gland. Review the reasons for the high rate of cell mitosis in the upper part of the intestinal gland.
216 Large intestine (Colon) View Virtual EM Slide
Goblet cells are particularly numerous in the large intestine. If you look closely at the labeled goblet cell, you can see that the apex is packed with mucus-containing secretory vesicles. A single crypt is seen in the section and its lumen doesn’t stay in the plane of section all the way to the base.
Click on a question to reveal the answer.
Note that the brush border is also PAS positive. Why?
The brush border is PAS positive both because of the glycocalyx that it contains and the pancreatic enzymes that stick to the glycocalyx.
How do the locations of glands in the GI tract help to identify what part of the GI tract you are looking at?
In the GI tract, the presence and appearance of glands can be very telling. Lets begin with the pharynx. The pharynx has no muscularis mucosa or submucosa and its glands can be found imbedded in layers of muscle beneath the epithelium. The esophagus is unique because it is one of two places in the gut where you will ever see submucosal glands. Stratified non-keratinizing squamous epithelium and glands in the submucosa (called esophageal glands proper) is characteristic of esophagus. In the stomach you can see various sized glands, all of which are located in the lamina propria, at the base of the gastric pits. These glands contain parietal, chief and enteroendocrine cells. The duodenum is the second place in the GI tract with submucosal glands (Brunner’s glands). Unlike the esophagus, however, the duodenum has villi and intestinal glands in the lamina propria, like the rest of the small intestine (the submucosal glands of the duodenum are of secondary importance to the glands found in the lamina propria). The presence or absence of submucosal glands is a key difference between duodenum and the rest of the small intestine. In the remainder of the small intestine, glands (crypts) are located at the base of the intestinal villi in the lamina propria. These glands contain Paneth cells (which secrete lysozyme) and enteroendocrine cells. The colon, on the other hand, has no villi and has straight glands which are made up of abundant mucus secreting goblet cells.
1. Where are the blood vessels located that when dilated cause rectal hemorrhoids?
- In the lamina propria
- in the muscularis mucosae
- In the submucosa
- In the muscularis externa
- In the adventitia
Answer
Correct answer 3. These blood vessels are part of the submucosa.
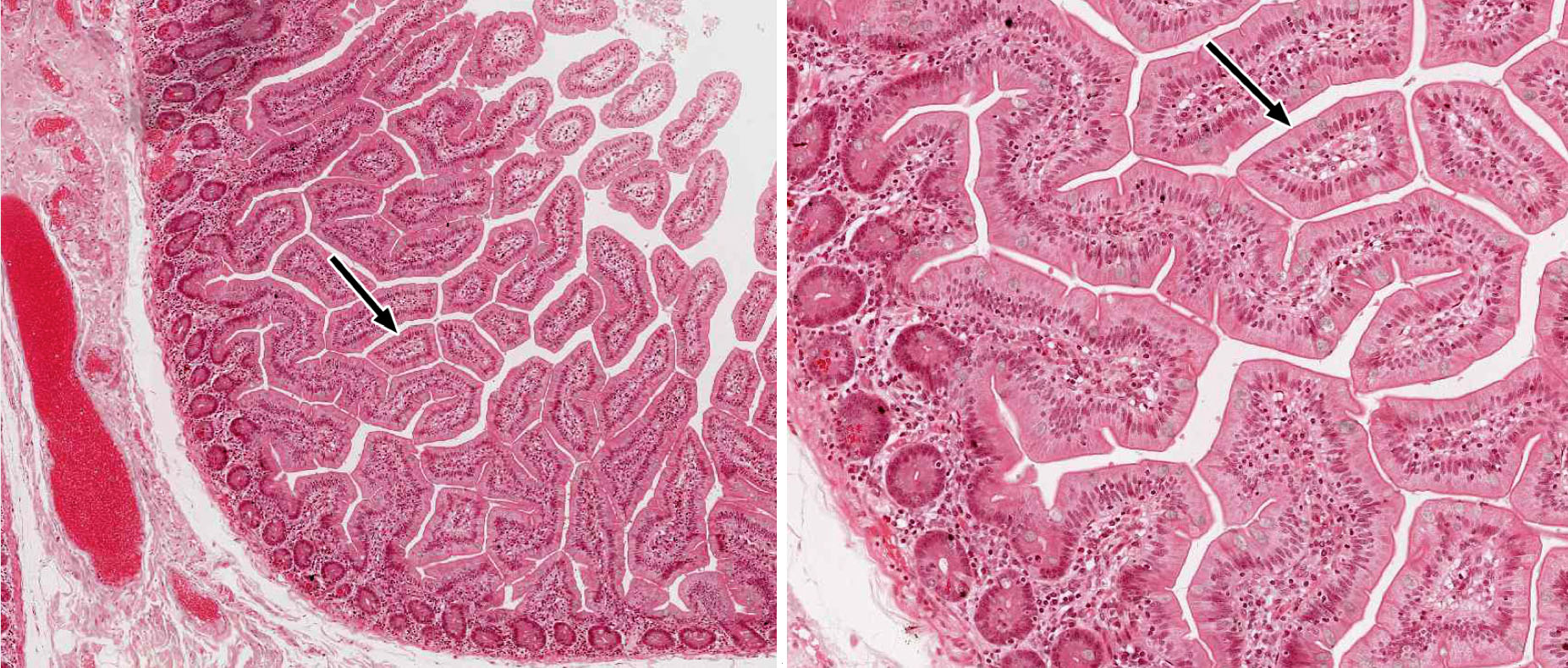
2. Identify the histological structure that is cut in cross section and marked by the black arrow.
- A gastric pit.
- A cardiac stomach gland.
- A fundic stomach gland.
- A pyloric stomach gland.
- A duodenal submucosal (Brunner’s) gland
- A villus in the jejunum/ileum
- A crypt of Lieberkühn in the jejunum/ileum.
- A crypt of Lieberkühn in the colon.
Answer
Correct answer 6. As the structure is surrounded by GI lumen, all answers containing glands or crypts can be eliminated. That only leaves a villus in the jejunum/ileum (note the absence of submucosal glands).
3. Identify the region of the GI tract from which this micrograph was obtained.
View Low Mag Image
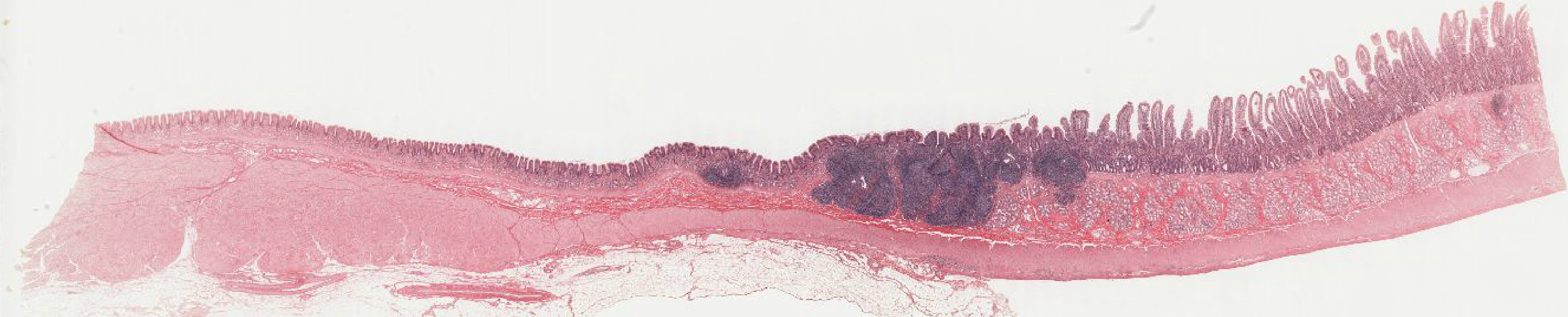
View Med Mag Image
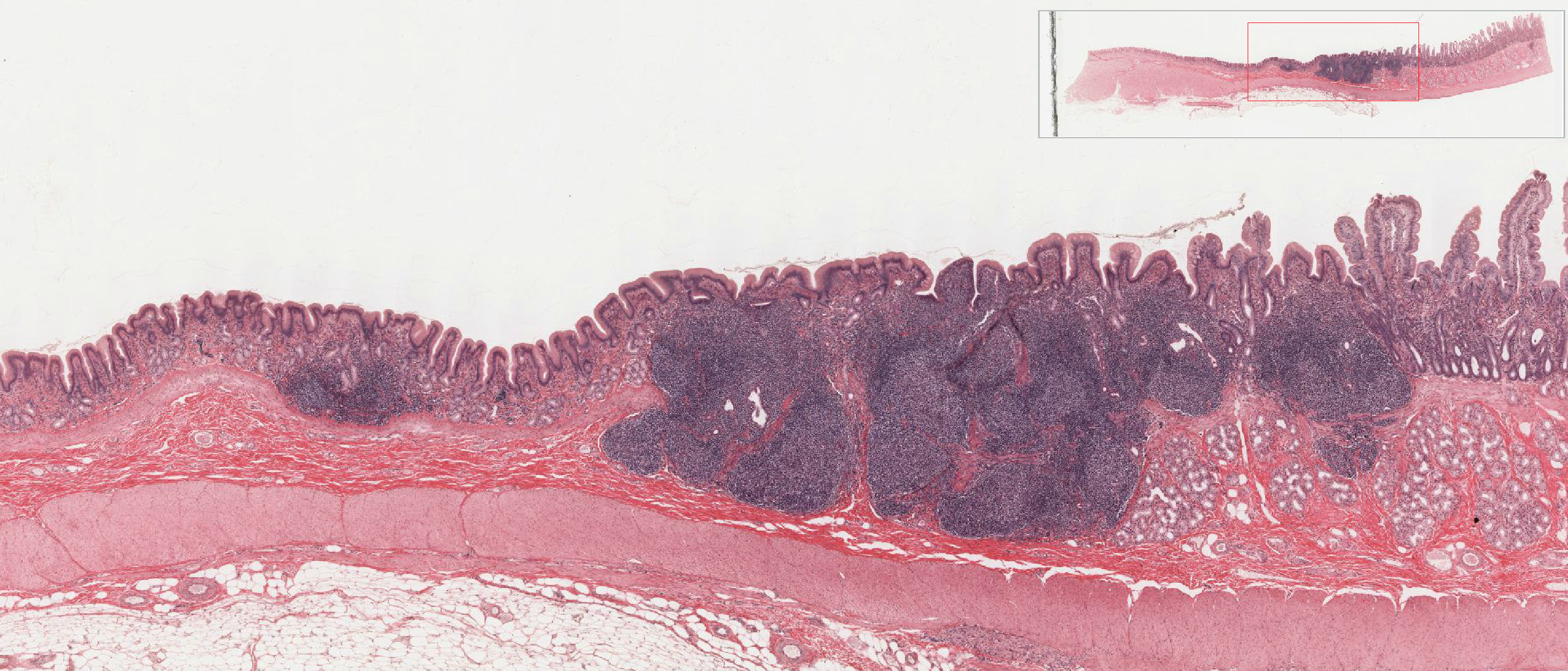
- The cardio-esophageal junction
- The gastro-duodenal junction
- The duodeno-jejunal junction
- The ileo-cecal junction
- The recto-anal junction
Answer
Correct answer 2. No change of epithelium is visible, eliminating answers 1. and 5. In contrast to the right side of the image, no villi are visible on the left side, eliminating answer 3. Submucosal glands on the right side identifies this as duodenum, leaving only 2. as the correct answer, the gastro-duodenal junction.
4. Identify the cells marked by the black arrows.
- They are fibroblasts of the lamina propria.
- They are smooth muscle cells of the muscularis mucosae.
- They are fibroblasts of the submucosa.
- They are neurons of the submucosal plexus.
- They are smooth muscle cells of the muscularis externa.
Answer
Correct answer 2. The shape and location of the marked cells suggests that these smooth muscle cells in the core of an intestinal villus. These smooth muscle cells are an extension and therefore part of the muscularis mucosae.