- Know the structural organization of the outer, middle and inner ear and what their respective functions are. Be able to recognize them at the light microscope and EM level.
- Be able to recognize and distinguish the auditory parts of the inner ear (cochlea, three different scalae, stria vascularis) from those of the vestibular system (saccules and utricles, maculae, semicircular canals, cristae ampullaris).
- Understand role of endolymph and perilymph and how they are involved in triggering hair cells.
- Know the location of the two different types of hair cells and be able to identify inner ear nerves (cochlear and vestibular) and ganglia (spiral and vestibular) in micrographs.
Slide 080a Ear cochlea H&E View Virtual Slide
Slide EAR-1 Ear petrous temporal bone H&E View Virtual Slide
Slide EAR-2 Ear petrous temporal bone H&E View Virtual Slide
Slide EAR-3 Inner ear inner ear H&E View Virtual Slide
Slide EAR-4 Ear petrous temporal bone View Virtual Slide
Embedded within the petrous portion of the temporal bone is the bony labyrinth which consists of the central vestibule, three semicircular canals, which arise and end at the vestibule, and the cochlea. It contains a fluid called perilymph, which has a composition similar to extracellular fluids (high in Na+, low in K+).
- Between the vestibule and middle ear is a tissue-covered hole in the bone, the “oval window”. The footplate of the stapes #EAR-3 View Image is attached to the oval window on the middle ear side. Here, vibrations of the tympanic membrane are converted into fluid vibrations of perilymph via the bones of the middle ear.
- The cochlea EAR-1 Ear petrous temporal bone H&E View Image, located anteriomedially to the vestibule consists of a tube spiraling around a bony axis (the modiolus).
The innervation of the cochlea and vestibule is as follows: The cell bodies of the cochlear neurons occupy a canal (the spiral canal) that spirals up the modiolus. This spiral aggregate of nerve cells is called the spiral (or cochlear) ganglion (see this Image for an orientation). Keep in mind that these are bipolar sensory neurons: their dendrites synapse with the hair cells in the organ of Corti (discussed below) and their axons come together in the cochlear nerve, which occupies a central canal in the modiolus and exits at the base of the cochlea. In the sensory regions of the vestibule, hair cells of the maculae and cristae (discussed below) synapse with dendrites of a corresponding aggregation of sensory neurons in the vestibular (or Scarpa's) ganglion (seen in #EAR-2 View Image, which then send their axons through the vestibular nerve. The processes of the vestibular nerve join with those of the cochlear nerve to form the vestibulocochlear nerve (cranial nerve VIII)Ear Image .
Some ancillary information:
Other neuroanatomical features of interest found within this region of the temporal bone in slide EAR-1 include the stapedius muscle #EAR-1 View Image, which is a thin bundle of skeletal muscle (innervated by the facial nerve) attached to the base of the stapes to dampen its movement. Also present is the facial nerve (cranial nerve VII) and, if the plane of section happens to be at the genu of the facial nerve, neuron cell bodies of the geniculate ganglion #EAR-1 View Image.
What is the function of the geniculate ganglion?
Answer
The geniculate ganglion is the sensory ganglion of the facial nerve and as such it contains sensory neurons that convey: taste from the palate and anterior 2/3 of the tongue; general somatic sensation from the external acoustic meatus; visceral afferent sensation from the palate and pharynx
The EAR-1 slide also shows some CNS tissue in the cranial vault #EAR-1 View Image; see if you can identify this organ.
Answer
Cerebellum --you should be able to identify the molecular layer, granular layer, and the very large Purkinje cells.
.
Slide 080a Ear cochlea H&E View Virtual Slide
Slide EAR-1 Ear petrous temporal bone H&E View Virtual Slide
Slide EAR-2 Ear petrous temporal bone H&E View Virtual Slide
Slide EAR-3 Inner ear inner ear H&E View Virtual Slide
Slide EAR-4 Ear petrous temporal bone View Virtual Slide
The membranous labyrinth consists of the interconnected utricle, saccule, three semicircular ducts, the endolymphatic duct and sac, and the cochlear duct. It contains a fluid, endolymph, much like intracellular fluid in composition (high K+, low Na+). You will not have difficulty recognizing the cochlear duct (scala media).
1. The utricle and the saccule contain the otolith organs that lie within the bony vestibule bony vestibule Image . These otolith organs consist of sensory areas called maculae , and you should note that they are oriented somewhat perpendicular to each other to be able detect movement in different planes. Taking a closer look at a macula (a really nice macula of the utricle is visible in #EAR-2 View Image, you should be able to identify the sensory epithelium comprised of hair cells and supporting cells (these can't be differentiated in the light microscope, but you should know the functions of each). It is overlaid by a gelatinous material (otolithic membrane) in which are embedded calcite crystals (otoliths or otoconia). The otoconia are quite visible in some slides, hardly visible in others. Beneath the sensory epithelium is a delicate connective tissue (filled with perilymph) and nerve fibers from the bipolar neurons of the vestibular (Scarpa's) ganglion. Note: you DO NOT need to be able to tell the macula of the utricle from the macula of the saccule, but you should be able to identify them as maculae in general and recall that maculae detect linear acceleration.
2. The semicircular ducts have dilations (ampullae) near their origins from the utricle. Each ampulla has a ridge of tissue, or crista ampullaris, (best seen in #EAR-2 View Image) that projects into the lumen. The crista has a sensory epithelium similar to that of the macula; recall, however, that the cristae are specialized to detect angular (or rotational) acceleration. The hairs of the hair cells project into a gelatinous material called the cupula. The cupula projects into the lumen more than the otolithic membrane of the macula, and lacks otoconia.
What would happen if any otoconia or other debris were to become lodged somewhere in a semicircular canal or in a cupula? Answer
Note that the "membrane" of the membranous labyrinth is suspended from the bone by a delicate connective tissue and that in the Ear-1 and Ear-2 slides this tissue has torn such that the membrane is now squished up against the crista, so there's not much of the cupula that can be seen Image.
3. The cochlear duct or scala media #EAR-1 View Image contains the organ of Corti, which detects sound (hearing). The cochlear duct is a triangular tube that is suspended in the middle of the spiraling bony labyrinth of the cochlea, thus subdividing this space into three spiraling sub-compartments, or “scalae”: the scala vestibuli, which opens on the vestibule; the scala media; and the scala tympani, which ends at the round window (the round window is not seen in any your slides). The scala vestibuli and scala tympani are both elements of the bony labyrinth and contain perilymph; the scala media or cochlear duct is an element of the membranous labyrinth and contains endolymph.
Elements of the cochlear duct that can be seen in cross section are: cochlear duct Image
- The vestibular membrane (also called Reissner’s membrane) is the tissue separating the cochlear duct from the scala vestibuli.
- The stria vascularis is a stratified epithelium along the outer wall of the cochlear duct that is unique in that it is vascularized (most epithelia are avascular) by an extensive capillary network --this is probably best shown in slide 80 #080a View Image; where you can see numerous profiles of capillaries containing RBCs. Cells of the stria vascularis are responsible for the production and maintenance of endolymph.
- The basilar membrane #EAR-1 View Image extends from the tip of the osseous spiral lamina of the central modiolus to the outer wall of the cochlea and separates the cochlear duct from the scala tympani. The organ of Corti rests on the basilar membrane.
Notice that the width of the basilar membrane changes such that it is shorter at the base and longer toward the apex of the cochlea. What is the significance of this change in length?Answer
The length of the basilar membranes determines its resonance frequency, or the frequency at which transduced sound waves will cause maximal displacement of the basilar membrane. Low-pitched sounds (low frequency sound waves) cause maximal deflection of the basilar membrane (and therefore maximal stimulation of the hair cells in the organ of Corti) toward the apex of the cochlea where the basilar membrane is longer. High-pitched sounds stimulate hair cells toward the base of the cochlea where the basilar membrane is shorter. Perhaps a bit silly, but here's a mnemonic: "It's low-nly at the top" (low pitched sounds stimulate hair cells at the top or apex of the cochlea).
- The organ of Corti #EAR-1 View Image consists of two kinds of hair cells and various supporting cells in a complex arrangement (NOTE: you may notice green lipid granules in some of the outer supporting cells, particularly toward the apex of the cochlea, in slide 80 --it's not a detail worth worrying about, but these support cells can change their mass and volume by altering the amount of lipid in their cytoplasm. The overall effect is a subtle change in the overall geometry of the organ of Corti and thus is a mechanism for fine tuning the sensitivity of the organ, particularly to low frequency sound).
The organ of Corti contains: organ of Corti Image
- The outer hair cells surrounded by outer phalangeal cells. There are three rows of outer hair cells. The apices of these cells and their phalangeal cells are joined together to form the reticular membrane (also called reticular lamina or apical cuticular plate) that separates endolymph in the scala media from underlying corticolymph and perilymph of the scala tympani. Lateral to the outer hair cells and phalangeal cells are other support cells, but you don't need to worry about knowing their specific types. Note that outer hair cells account for only ~5-10% of the sensory input into the auditory system. The primary function of outer hair cells is actually to contract when stimulated, thus "pulling" on the tectoral membrane thereby stimulating the inner hair cells.
- Outer and inner pillar cells outline a triangular shaped tunnel, called the inner tunnel, which is filled with perilymph-like fluid called corticolymph.
- The inner hair cells are in a single row close to the inner pillar cells (you may see more than one inner cell nucleus because of the thickness of the section). Note that the inner hair cells account for ~90-95% of the sensory input into the auditory system.
- The organ of Corti is overlaid by a gelatinous tectorial membrane (produced and maintained by the columnar cells found atop the spiral limbus just medial to the organ of Corti).
- Nerve fibers enter the organ of Corti through openings in a shelf of bone extending from the modiolus like the thread of a screw. The nerve fibers pass between supporting cells to synapse with the hair cells.
Compare the innervation and function of the inner vs. outer hair cells.Answer
Inner and outer hair cells have synapses with both afferent and efferent fibers, but at very different proportions. Inner hair cells account for about 90% of the INPUT into the auditory system, so they synapse mostly with afferent fibers from neurons of the spiral ganglion. The primary function of inner hair cells is SENSORY: they detect deflection of the basilar membrane. Outer hair cells are mostly innervated by efferent fibers (i.e. output from the CNS, particularly the medial superior olivary nucleus, to the cochlea), and they have the ability to contract when stimulated (either by deflection of their stereocilia caused by movement of the basilar membrane or from these efferent synapses). The primary function of outer hair cells is, therefore, MODULATORY: contraction/relaxation of the outer hair cells affects overall movement of the basilar membrane and essentially "tunes" the organ of Corti to be more or less sensitive to particular sound frequencies.
A few notes about deafness: Disruption of any part of the process by which sound waves are transduced into input into the auditory portion of the CNS will result in "deafness." Damage to the eardrum or ossicles results in so-called "conduction" deafness whereby sound waves are no longer transmitted into the inner ear. In this instance, a patient would NOT be able to hear a tuning fork held near the pinna, and the loss of hearing would extend across the entire range of frequencies. However, placing the stem of the fork on a bony part of the skull (e.g. the mastoid process) would then transmit vibrations directly to the inner ear (via the bone) where they could then be "heard."
Loss of components within the cochlea results in sensorineural deafness which is more frequency-specific (i.e. the patient will not be able to hear specific pitches depending on the location of the damage in the cochlea). Loss of OUTER HAIR CELLS in a particular region of the cochlea would result in a "threshold shift" whereby sound of a particular frequency could still be detected (because the inner hair cells are still intact), but it would have to be LOUDER to make up for the fact that there are no outer hair cells to help stimulate the inner hair cells. This type of hearing loss can be compensated by a hearing aid.
Loss of INNER HAIR CELLS in a particular region of the cochlea would result in an almost complete inability to detect specific frequencies regardless of how loud they are. Loss of SPIRAL GANGLION CELLS would have a similar effect since these are the cells that actually project into the CNS. In both cases, the deafness could only be corrected with a cochlear implant.
337 Organ of Corti View Virtual EM Slide
Note the position of inner and outer hair cells in the Organ of Corti. Also know, which spaces are filled with perilymph and with endolymph, respectively.
Click on a question to reveal the answer.
What is the function of the geniculate ganglion?
The geniculate ganglion is the sensory ganglion of the facial nerve and as such it contains sensory neurons that convey: taste from the palate and anterior 2/3 of the tongue; general somatic sensation from the external acoustic meatus; visceral afferent sensation from the palate and pharynx
Notice that the width of the basilar membrane changes such that it is shorter at the base and longer toward the apex of the cochlea. What is the significance of this change in length?
The length of the basilar membranes determines its resonance frequency, or the frequency at which transduced sound waves will cause maximal displacement of the basilar membrane. Low-pitched sounds (low frequency sound waves) cause maximal deflection of the basilar membrane (and therefore maximal stimulation of the hair cells in the organ of Corti) toward the apex of the cochlea where the basilar membrane is longer. High-pitched sounds stimulate hair cells toward the base of the cochlea where the basilar membrane is shorter. Perhaps a bit silly, but here's a mnemonic: "It's low-nly at the top" (low pitched sounds stimulate hair cells at the top or apex of the cochlea).
Compare the innervation and function of the inner vs. outer hair cells.
Inner and outer hair cells have synapses with both afferent and efferent fibers, but at very different proportions. Inner hair cells account for about 90% of the INPUT into the auditory system, so they synapse mostly with afferent fibers from neurons of the spiral ganglion. The primary function of inner hair cells is SENSORY: they detect deflection of the basilar membrane. Outer hair cells are mostly innervated by efferent fibers (i.e. output from the CNS, particularly the medial superior olivary nucleus, to the cochlea), and they have the ability to contract when stimulated (either by deflection of their stereocilia caused by movement of the basilar membrane or from these efferent synapses). The primary function of outer hair cells is, therefore, MODULATORY: contraction/relaxation of the outer hair cells affects overall movement of the basilar membrane and essentially "tunes" the organ of Corti to be more or less sensitive to particular sound frequen
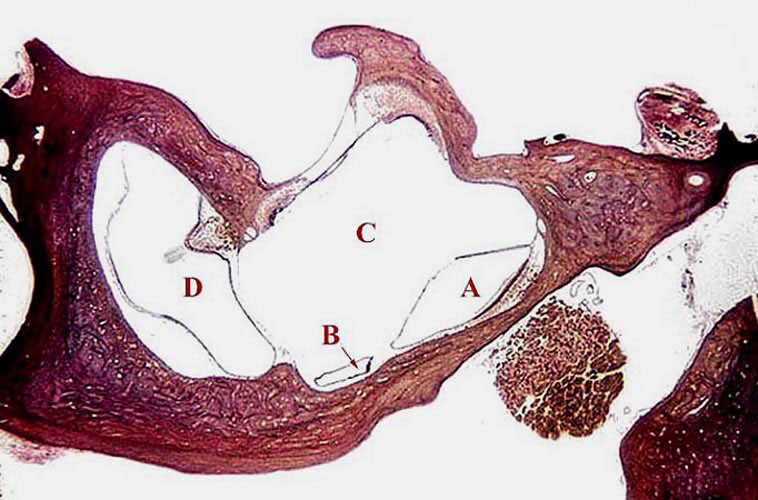
1. Which letter in in a semicircular canal?
- A
- B
- C
- D
Answer
Correct answer 4. (D). Note the clearly visible ampulla. A and B indicate otolith organs (B is probably the macula whereas A is probably the saccule, but remember that you are not expected to differentiate between the two). C is in the perilymph-filled space of the vestibule.
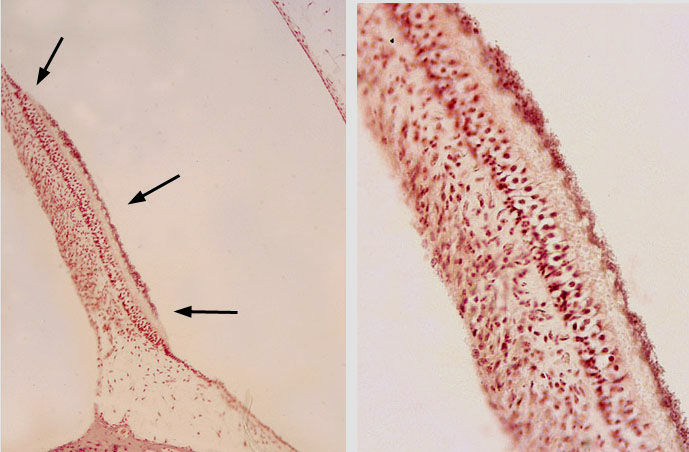
2. Which statement about the structure indicated by the arrows in the left panel and shown at a higher magnification in the right panel is correct?
- produces endolymph.
- detects angular acceleration.
- detects linear acceleration.
- detects low frequency sound.
- detects high frequency sound.
Answer
Correct answer 3. The marked structure is a macula or otolith organ (note the otoliths) which detects linear acceleration.
3. The cells marked by the red arrow form synaptic contacts with which of the following cells?
View Image
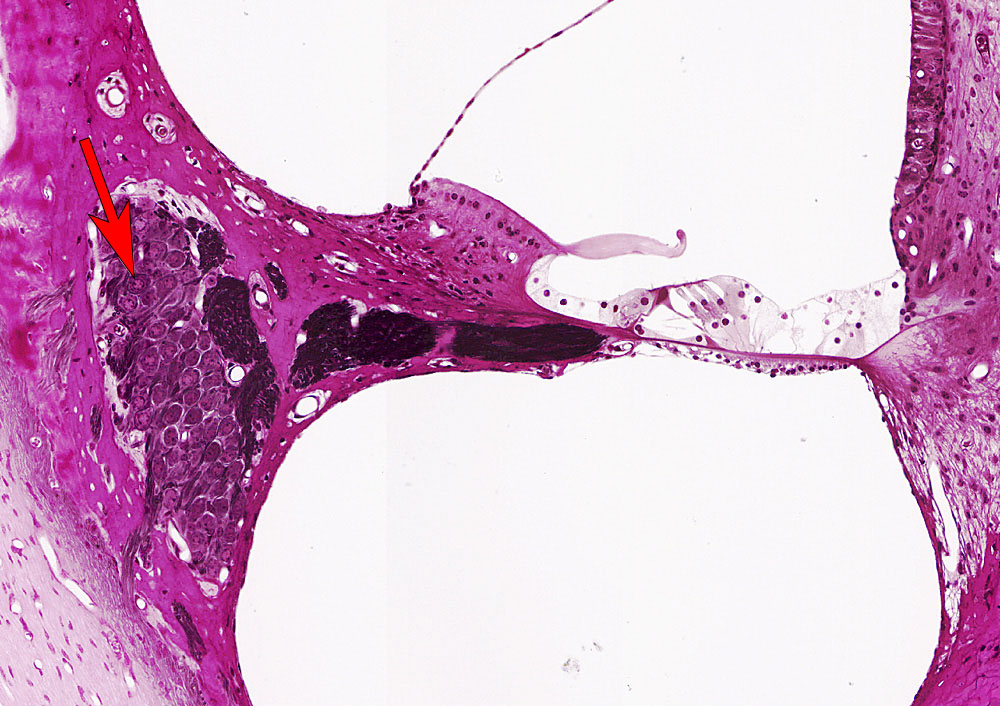
- Sensory neurons of the vestibular (Scarpa's) ganglion
- Sensory neurons of the geniculate ganglion
- Hair cells in a crista ampullaris
- Hair cells in an otolith organ
- Hair cells in the organ of Corti
Answer
Correct answer 5. The neurons of the spiral ganglion make synaptic contact with hair cells in the organ of Corti. These spiral ganglion cells are the 1st-order sensory neurons of the auditory system.
4. Which statement(s) about perilymph is/are correct?
- It is extracellular fluid that fills the bony labyrinth.
- It has a high concentration of Na+ ions and a low concentration of K+ ions.
- It normally contains very little plasma proteins such as albumin.
- It is in direct contact with the oval window.
- ALL of the above statements are correct.
- None of the above statements is correct.
Answer
Correct answer 5. ALL of the above statements are correct.