- Be able to describe the main layers of the digestive tract wall (mucosa, submucosa, muscularis externa, and adventitia/serosa), and know how they differ in the pharynx, esophagus, and stomach.
- Know the three layers of the gastrointestinal mucosa and be able to recognize them in micrographs (epithelium, lamina propria, and muscularis mucosae).
- Know the histological differences in the pharynx and the upper, middle, and lower segments of the esophagus.
- Understand the histological structure of the stomach mucosa (including pits and glands).
- Be able to recognize gastric glands, identify their main constituent cells (parietal and chief cells), and know their respective secretory products.
- Be able to differentiate cardiac, body/fundus, and pyloric regions of the stomach.
The wall of the gastrointestinal tube consists of 4 major layers (W pgs 263-266): the mucosa, the submucosa, the muscularis (also called muscularis propria or muscularis externa) and the serosa (if covered by peritoneum) or adventitia (if retroperitoneal). The mucosa, in turn, consists of an epithelium, a supporting lamina propria of loose connective tissue and a thin, usually double, layer of smooth muscle, themuscularis mucosae. The four major layers will be examined in each region of the digestive system. The mucosa differs considerably from region to region, reflecting changing functional activity. Be sure to identify these differences. The other layers in the wall change rather little, although there are subtle differences also in these layers that can also help you identify particular regions of the GI tract.
To help you keep track of changes in the various layers, you can fill in this spreadsheet as you work through today's and next week's labs.
Slide 152 40x (H&E) View Virtual Slide
Slide 152 triC (aldehyde fuchsin) View Virtual Slide
The oral pharynx is lined by a stratified squamous non-keratinizing type of epithelium and lacks both muscularis mucosae and submucosa. The epithelium rests on a lamina propria that contains a thick layer of longitudinally oriented elastic fibers (a useful diagnostic feature). The fibers, which stain deep purple with aldehyde fuchsin, are readily recognized in slide 152AF whereas in the H&E-stained slide the elastic fibers appear dark, glassy red. Note that these fibers are located in the lamina propria near the underlying muscularis externa. The muscularis externa is composed of somewhat irregularly arranged skeletal muscle, the longitudinal and constrictor muscles of the pharynx. Mucous glands seen in this muscular layer in some of our glass slides are the extensions of those present in the lamina propria. The outer fibrous layer, which connects the pharynx to the adjacent structures, is not included in many of your slides.
Slide 126 40x (trachea & esophagus, H&E) View Virtual Slide
Slide 153 20x (esophagus, H&E) View Virtual Slide
Slide 155 40x (gastro-esophageal junct, H&E) View Virtual Slide
For the purpose of histological descriptions, the esophagus is subdivided into upper (entirely skeletal muscle in the muscularis externa),middle (mixed smooth and skeletal muscle) and lower (entirely smooth muscle) portions. We don't have any slides showing purely upper esophagus, but you can use slides 126 (mid-upper), 153 (mid-lower) and 155 (esophageal-cardiac junction) to study the basic histology and regional variations of the esophagus. The esophageal epithelium View Image is the non-keratinized stratified squamous type and is supported by a connective tissue lamina propria. Note the presence of isolated lymphoid nodules View Image and scattered leukocytes in the lamina propria. In additiona to the characgteristic submucosal glands of the esophagus, small mucous glands may be found scattered in the lamina propria of the upper and lower esophagus in some of our glass slides. A rather thick layer of longitudinally arranged smooth muscle fibers form the muscularis mucosae View Image. The connective tissue of the submucosa consists of mostly collagenous fibers with some elastic fibers and varying amounts of fat as well as submucosal sero-mucous glands which can be readily observed in both slide 126 View Image and slide 153 View Image (those in slide 155 are not very well preserved).
In the upper esophagus, the muscularis externa consists of both inner and outer layers of skeletal muscle only. In the middle esophagus, the muscularis externa contains a mixture of skeletal and smooth muscle as seen in slide 126 View Image, whereas in the lower esophagusonly smooth muscle is found as seen in slide 155 View Image. Present in all regions of the esophagus (upper, mid, and lower) is the myenteric (Auerbach’s) plexus View Image between the two layers of the muscularis externa. For most of its extent, the esophagus is retroperitoneal, so its outermost layer consists of a connective tissue adventitia which merges with the adjacent connective tissue associated with nearby structures (such as the trachea as shown in slide 126). Below the diaphragm, however, the esophagus is suspended within abdominal cavity and is therefore covered by a connective tissue serosa as shown in slide 155.
General Characteristics: The stomach is divided into four regions: the cardia, fundus, corpus (body) and pylorus. The wall of the stomach consists of the usual four layers present in other parts of the gastrointestinal tract. The mucosa is relatively thick and contains numerous tubular glands. The muscularis mucosae is also thick and, in some areas, it consists of 3 layers of smooth muscle, although this layering is not always visible. Glands are absent in the submucosa. In the empty contracted stomach, the mucosa is thrown into longitudinal folds (rugae) because of the contraction of the muscularis mucosae and the loose consistency of the submucosa. The surface is further subdivided by furrows, the gastric pits. These funnel-shaped invaginations of the epithelium are continuous at their base with the tubular glands. The muscularis externa is made up of 3 ill-defined layers. The middle circular layer of the muscularis is thickened to form thepyloric sphincter, which is an “anatomic” sphincter. The lower (gastro-)esophageal sphincter does not have this thickening of the muscularis, so this is why it is called a “physiological” sphincter.
On the basis of differences in the types of glands present in the mucosa, three histological regions can be distinguished in the stomach. The first region around the cardia contains the cardiac glands. The second region, which includes the fundus and corpus, contains the gastric glands proper (also called fundic glands). The distal region of the stomach (pylorus) contains pyloric glands.
A. Cardiac glands (W pg 268, 14.6)
Slide 155 40x (gastro-esophageal junct, H&E) View Virtual Slide
Slide 160 40x (gastro-esophageal junct, PAS & Azure Blue) View Virtual Slide
These mucosal glands are composed mainly of mucous cells with pale staining cytoplasm and basally located nuclei. Present, but not seen, are stem cells and endocrine cells. In slide 155, locate the cardio-esophageal junction (W pg 268, 14.6) View Image. Note the abrupt transition from the mucosa of the esophagus with its stratified squamous epithelium to the glandular mucosa of the stomach. The cardiac gastric glands View Image are present only in a very small segment of the stomach mucosa adjacent to this junction. They are mucous glands comprised of a HOMOGENEOUS population of pale-staining columnar cells with a “bubbly” supranuclear cytoplasm. As you move further into the stomach, the cardiac glands are very quickly replaced by gastric proper (or fundic) glands which, as described below, consist of a notably HETEROGENEOUS mixture of basophilic chief cells and eosinophilic parietal cells.
Since the cardiac gastric glands are primarily mucous, they can also be be demonstrated with the PAS stain, as shown in slide 160. In this slide, the cells lining the gastric pits View Image stain very intensely with PAS due to the carbohydrate-rich, viscous mucus they secrete. The secretion of the cardiac glands is a bit more watery so they do not stain quite as intensely.
B. Gastric glands (W pg 268-272, 14.7-13).
Slide 155 40x (gastro-esophageal junct, H&E) View Virtual Slide
Slide 160 40x (gastro-esophageal junct, PAS & Azure Blue) View Virtual Slide
Slide 156 20x (stomach, H&E) View Virtual Slide
Slide 156 40x (stomach, H&E) View Virtual Slide
Slide 157 20x (stomach, H&E) View Virtual Slide
Slide 157 40x (stomach, H&E) View Virtual Slide
"Gastric" or "fundic" glands are characteristic of the mucosa throughout the fundus and corpus regions of the stomach. At low magnification, notice that the gastric pits are relatively more shallow here View Image and the tubular gastric or fundic glands are relatively much longer than those in the cardia or pylorus. Observe that the tall columnar cells lining the luminal surface and pits have basally located nuclei and lightly staining cytoplasm. Most of these cells secrete mucus, that is stored in the apical cytoplasm. You can see these cells in the stomach preparation stained with PAS (which will stain mucus and other glycoproteins) in slide 160. In this slide, the mucous cells of the gastic pits stain quite intensely. Also identifiable are lighter-staining "mucous neck cells" present in the neck region of the gastric glands and mucus-secreting cells of the cardiac glands found near the gastro-espophageal junction.
Moving into the body of a fundic gland, identify the parietal and chief cells in slides 155 View Image [ORIENTATION], slide 156 View Image [ORIENTATION], and slide 157 View Image [ORIENTATION]. Parietal cells are large, ovoid to pyramidal shaped cells with their broad side adjacent to the basement membrane. Each cell contains a round, centrally located nucleus and reveals a lightly eosinophilic cytoplasm that appears granular due to the presence of many mitochondria. The chief cells are present in the lower one-third to one-half of the gastric glands. The apical cytoplasm of these cells may appear granular due to the presence of zymogen granules, that may stain bright red in H&E preparations (as in slide 157). However, in other preparations (slides 155 and 156), the pepsinogen has been extracted and the empty secretory granules resemble many glass beads in the supranuclear cytoplasm. The base of the cytoplasm, on the other hand, is distinctly basophilic.
Other cells of the gastric glands, such as undifferentiated (stem) cells and various endocrine cells, will NOT be studied in this laboratory session as they are not readily identifiable in the stomach, but you should be aware of their general characteristics. Notice the presence of a large number of lymphocytes and plasma cells in the lamina propria between the gastric glands, and, in some areas, aggregated as lymphoid nodules View Image (which will be studied in greater detail along with other lymphatic tissues but you should at least be able to identify them here). Also, notice that the strands of smooth muscle fibers from the inner layer of the muscularis mucosae extend between the glands toward the surface. The contraction of these strands may help the emptying of the glands.
C. Pyloric glands (W pgs 273, 14.14-15)
Slide 162 20x (gastro-duodenal junct, H&E) View Virtual Slide
Slide 162 40x (gastro-duodenal junct, H&E) View Virtual Slide
In slide 162, you can see the transition from pylorus of the stomach to duodenum of the small intestine. The pyloric region of the stomach is characterized by a thick wall due to the presence of the pyloric sphincter muscle View Image, which is comprised primarily of the inner circular layer of the muscularis externa. Compare its wall thickness with that of the adjacent duodenum (W pg 273, 14.15). The pyloric glands View Image at the base of each gastric pit [ORIENTATION] are also composed again of a mostly HOMOGENEOUS population of mucous cells that are similar in appearance to those in cardiac glands although the pits are much deeper compared to cardiac glands. Present, but not seen, are stem cells and endocrine cells. An occasional parietal cell may be also found. Note that the bases of the pyloric glands abut the muscularis mucosae whereas in the duodenum, you will see abundant glands (Brunner's glands) DEEP to the muscularis mucosae (i.e. in the SUBMUCOSA).
Just in case you are worried about identifying cardiac glands versus pyloric glands, it is admittedly very difficult to tell these two apart based only on high-mag views, but you can always use contextual information to help you out: cardiac glands will be right near the gastro-esophageal junction whereas pyloric glands are at the gastro-duodenal junction.
190 Esophagus - Stratified Squamous non-keratinized epithelium View Virtual EM Slide
Compare this micrograph to EM#65. This is the lining of the esophagus, where it is no longer necessary to have an outer keratinized layer to protect against desiccation, as it was for skin. Thus, the outermost layer is still cellular and contains a nucleus. Note again the spiny appearance of the cells, due to the desmosomal attachments.
197 Stomach - Fundus Stomach - Gastric Pits and Glands View Virtual EM Slide
Note that there is only one cell type, a mucous cell, in the surface epithelium of the stomach. The gastric pits lead into the gastric glands proper, where there are several cell types present. As always, the lamina propria consists of loose connective tissue. There is a rich capillary network in the lamina propria.
198 Stomach - Mucous Surface Cell View Virtual EM Slide
Mucous Surface Cell (Stomach Fundus). Mucous (mucigen) granules accumulate in the apical cytoplasm before they are released.
203 Stomach - Chief Cell Chief Cell (Stomach Fundus) View Virtual EM Slide
Review the structure of the chief cell. It is essentially that of an exocrine gland cell - as seen in the salivary glands and the pancreas. What is(are) their secretory product(s)? (DG3).
204 Stomach - Parietal Cell Parietal Cell (Stomach Fundus) View Virtual EM Slide
Note the abundant vesicles and tubules of the parietal cell, which are involved in HCl production. Note the numerous giant mitochondria in the parietal cell as opposed to the small and sparse mitochondria in the chief cells. Study the intracellular secretory canaliculi of the parietal cell.
205 Stomach - Enteroendocrine Cell View Virtual EM Slide
Note the accumulation of secretory vesicles in this enteroendocrine cell. They are usually found adjacent to the basal and lateral sides of the cell, not the apical aspect, which is facing the lumen of the gastrointestinal tract. You will not be asked to discriminate between different subtypes of enteroendocrine cells.
Click on a question to reveal the answer.
What causes the basophilia in the basal cytoplasm of a chief cell?
The basophilic materials represent a large amount of rough endoplasmic reticulum present in this region of the cytoplasm, a characteristic appearance of a cell very active in protein synthesis.
What is(are) the secretory product(s) of chief cells?
Chief cells secrete pepsinogen, the precursor of the proteolytic enzyme pepsin.
1. Identify the type of glands that is depicted in the below micrograph.
- Esophageal submucosal glands
- Esophageal mucosal (i.e. "cardiac") glands
- Cardiac stomach glands
- Fundic (gastric) glands
- Pyloric glands
Answer
Correct answer 4. The image depicts fundic (gastric) glands. Note the abundance of parietal and chief cells.
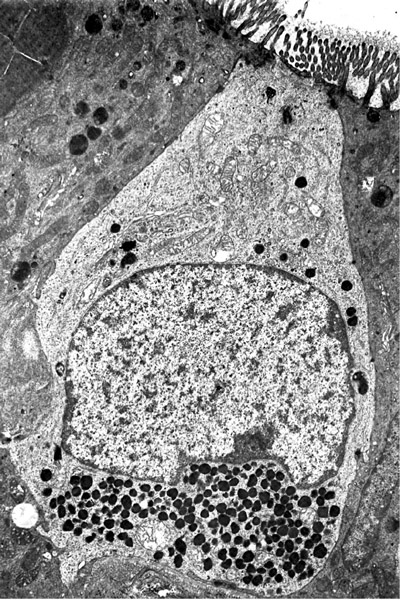
2. Which statement(s) is/are true about the cell depicted in this EM micrograph?
- This cell influences motility and secretory activity of the GI tract.
- This cell protects the mucosa by secreting mucus.
- This cell produces zymogens, such as pepsinogen, that are essential for digestion.
- This cell secretes intrinsic factor that is necessary for the absorption of vitamin B12.
- This cell secretes H+ ions for the production of acidic gastric juices.
Answer
Correct answer 1. Notice the basal secretory granules. This EM depicts an end-endocrine cell. Among other functions these cells influence the motility and secretory activity of the GI tract.
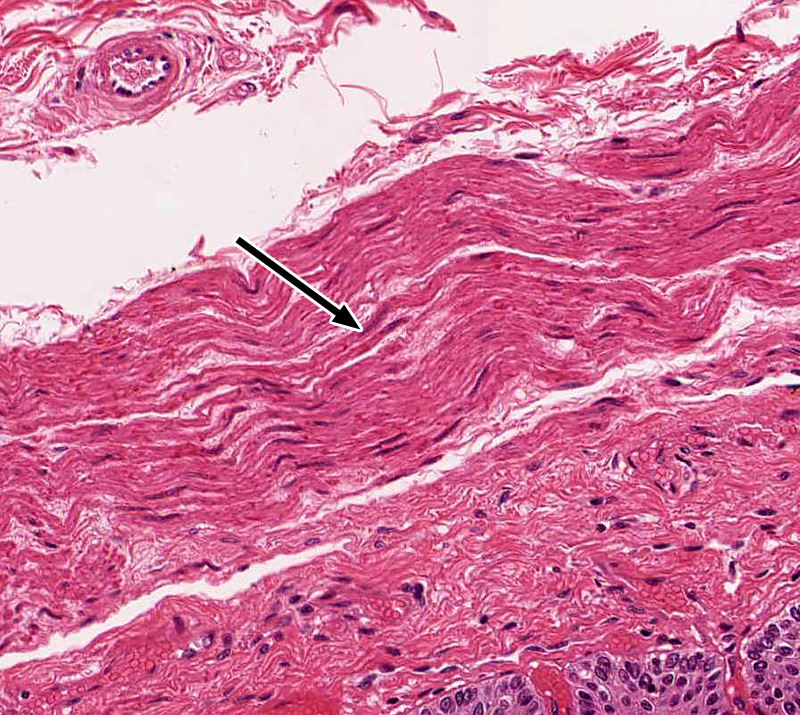
3. Which histological structure is indicated by the black arrow?
- The lamina propria of the esophagus
- The muscularis mucosae of the esophagus
- The submucosa of the esophagus
- The muscularis externa of the esophagus
- The lamina propria of the pharynx
Answer
Correct answer 2. As the arrow points to a layer of smooth muscle cells located below a stratified squamous non-keratinized epithelium, it is the muscularis mucosae of the esophagus. The pharynx has no muscularis mucosae and the muscularis external is visible in the left upper corner of the low magnification image.
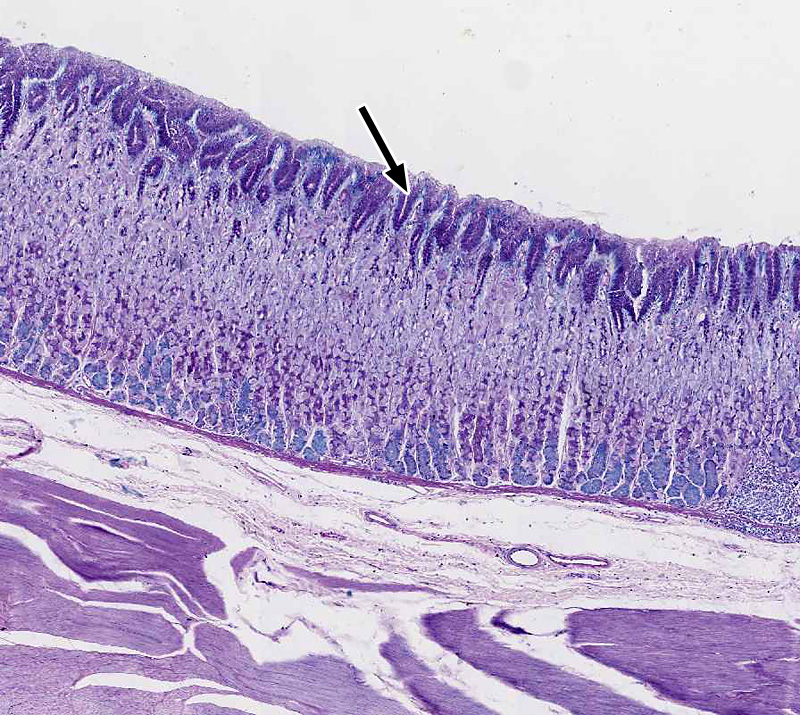
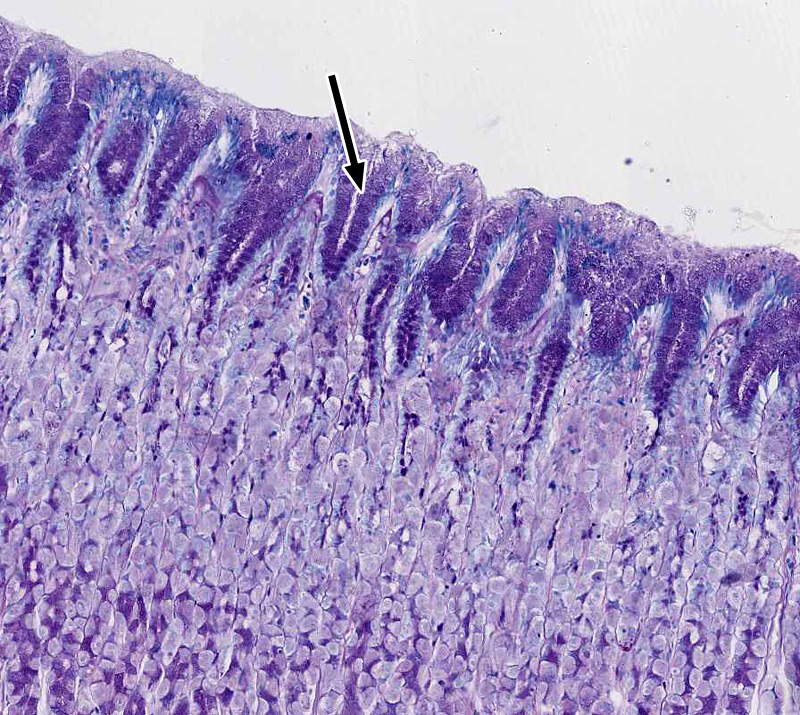
4. This tissue section was stained with PAS and Azurell stain. Which statement(s) is/are true about the cells marked by the black arrow?
- They secrete a watery mucus when stimulated by the vagus nerve.
- They are only found in the fundus/corpus of the stomach.
- They secrete H+ ions for the production of acidic gastric juices.
- They constitutively secrete a thick, bicarbonate-rich mucus.
- They produce zymogens such as pepsinogen essential for digestion.
Answer
Correct answer 4. The stain highlights mucus-secreting cells. The cells marked are epithelial cells that line the pits of the stomach fundus/corpus. They constitutively secrete a thick, bicarbonate-rich mucus.