Cartilage
- Be able to recognize and differentiate the three major cartilage types (hyaline, elastic and fibrocartilage) in light microscope images and know how they differ in composition and examples where each type is found in the human body.
- Be able to identify cells and structures in a cartilage microscopic section (e.g., chondroblasts, chondrocytes, lacunae, isogenous groups, territorial and interterritorial matrix, and the perichondrium).
- Know the major components of cartilage matrix and understand how they are responsible for cartilage resilience.
- Understand the two types of cartilage formation in adults (appositional and interstitial growth) and the role of mesenchymal stem cells in the perichondrium.
- Know about the regenerative potential of different types of cartilage and how the cartilage matrix changes with age.
hyalos = glass (Greek)
Slide 020 trachea connective tissue fibroblast plasma cell H&E View Virtual Slide
Slide 040 trachea H&E View Virtual Slide
Slide 040N hyaline cartilage 1.5um section H&E View Virtual Slide
Slide 126 trachea, esophagus H&E View Virtual Slide
These slides are good examples of mature hyaline cartilage with its abundant matrix and spaces, lacunae, occupied by cells, chrondocytes, which usually shrink extensively during fixation. The staining of the matrix is variable. Remember that there are abundant type II collagen fibrils in the matrix. However, they are too small to be resolved in the light microscope, so the matrix has an amorphous, glassy (or "hyaline") appearance. The predominately basophilic staining of the matrix in slide 126 reflects preservation of the negatively charged aggrecan molecules in the matrix. Note that the basophilia varies and some interterritorial matrix is eosinophilic reflecting loss (or minimal content) of negative charges, whereas the territorial matrix (the area immediately surrounding each lacuna) is much more basophilic. The differential staining of the territorial matrix compared to the interterritorial matrix is perhaps best shown in slide 040N. The staining actually reflects the relative content of aggrecan. Try to find an area where the cartilage has not pulled away from its investing fibrous perichondrium. In regions where there is no separation, you can see the stages of chondroblast entrapment slide 040 View Image into the matrix (arrested at this point, the cartilage is no longer growing) and the eventual enlargement and rounding of the lacunar space. Look for cell clusters, isogenous groups. For more practice in recognizing hyaline cartilage, look at the nasal septum in slide 124 View Virtual Slide.
Slide 044 Ear pinna Masson View Virtual Slide
Slide UCSF 053 ear pinna View Virtual Slide (virtual slide courtesy of the University of California, San Francisco)
Slide 044H epiglottis H&E View Virtual Slide
Slides 044 and UCSF 053 are from the pinna of the ear stained with aldehyde fuchsin and Masson's trichrome (slide 044) or elastic van Gieson's stain (UCSF 053). In slide 044 stained with aldehyde fuchsin, note the extensive, dark purple elastic fiber network within the cartilage matrix. In slide 053, the elastic fibers stain black whereas the rest of the matrix is yellow-brown. Elastic cartilage can be readily identified in routine H&E sections as well as shown in slide 044H which is from the epiglottis. Look for the plates of elastic cartilage found just under the glands deep to the respiratory epithelium. Observe that there are chondrocytes within lacunae just as in hyaline cartilage, but note the eosinophilic, fibrillar matrix due to the presence of elastic fibers. As with hyaline cartilage, fibrils of type II collagen are present, but they cannot be seen in the light microscope. You may also notice that elastic cartilage tends to be more cellular than hyaline cartilage. You can only convincingly identify the elastic cartilage when the section is specifically stained for elastin.
Slide 045 Intervertebral disc H&E View Virtual Slide
This cartilage is named for its textured matrix; it looks fibrous, and in addition lacunae can be seen. Locate the nucleus pulposus (clear area) of the intervertebral disc, then move out to the edge of the section to see fibrocartilage slide 045 View Image. Note the fibrous texture of the matrix due to the presence of type I collagen fibers in addition to the type II collagen present in all cartilage tissue (type II fibrils are not bundled into fibers large enough to be visible in the light microscope), but note also the distinct chondrocyte lacunae. Also, note that there is no perichondrium in this cartilage.
75 Hyaline Cartilage View Virtual EM Slide
Note the abundance of intercellular matrix. Are capillaries present in the matrix? (CA2) Study the development of chondrocytes from chondroblasts.
76 Cartilage - Chondrocyte (Hyaline Cartilage) View Virtual EM Slide
Note that the collagenous fibrils are partially obscured and lack obvious periodicity. What type of collagen is found in the matrix? (CA3) Note the many cell organelles, such as ribosomes, in this very active chondrocyte.
78 Chondrocyte (Fibrocartilage) View Virtual EM Slide
This low power electron micrograph nicely depicts the typical appearance of fibrocartilage as found in the intravertebral disk.
79 Cartilage - Chondrocyte (Fibrocartilage) Cartilage - Chondrocyte (Fibrocartilage) View Virtual EM Slide
Extracellular collagenous fibrils are coarser in fibrous cartilage than in hyaline cartilage and do show periodicity. They are made of type I collagen. Observe the varied directions of collagenous bundles. The amorphous matrix surrounding the chondrocyte helps distinguish this cell from that of a fibroblast in dense connective tissue.
82 Elastic Cartilage - Chondrocyte Detail View Virtual EM Slide
Find the elastic components in the matrix.
Click on a question to reveal the answer.
How would differences in the relative content of aggrecan affect cartilage function?
Since aggrecan molecules are negatively charged, they are basophilic. The difference in basophilic staining reflects the relative content of glycosaminoglycan (aggrecan). The glycosaminoglycans are highly negatively charged and highly hydrophilic and occupy a hugh volume relative to their mass. The high density of negative charges attracts cations, such as Na+, that are osmotically active, causing a large amount of water to be sucked into the matrix. This creates a swelling pressure, or turgor, that enables the matrix to withstand compressive forces. Cartilage matrix resists compression by this mechanism. A loss of aggrecan would lead to a reduction of turgor in the cartilage and weaken it.
Are capillaries present in the matrix?
Cartilage is an avascular tissue.
What type of collagen is present in hyaline cartilage matrix?
Hyaline cartilage contains fibers made primarily of type II collagen only. Fibrocartilage contains type II collagen but also contains abundant type I collagen. Elastic cartilage contains type II collagen and elastic fibers.
1. Identify the true statement(s) about the type of cartilage shown in this micrograph.
View Image
- It is highly resistant to compression.
- It is ALWAYS completely invested by a fibrous perichondrium.
- It contains a matrix of type I collagen fibers and hyaluronan.
- It is found primarily in the pinna of the ear and the epiglottis.
- ALL of the above statements are true.
Answer
Correct answer 1. Hyaline cartilage is highly resistant to compression. It does NOT always have a perichondrium (as in articular cartilage). Its matrix consists of type II collagen and hyaluronan, and it is NOT found in the pinna of the ear and epiglottis (elastic cartilage is found there).
2. Which of the following statement(s) is/are true about fibrocartilage?
- It is present in intervertebral disks.
- It usually inserts into bone.
- It contains a matrix of type II collagen and hyaluronan.
- It has high tensile strength.
- ALL of the above.
Answer
Correct answer 5. All of the statements are TRUE. Note that statement 3 is TRUE. The matrix of fibrocartilage does contain type II collagen and some hyaluronan (of course, there's also a lot of type I collagen (just because type 1 collagen wasn't mentioned does NOT make the statement incorrect).
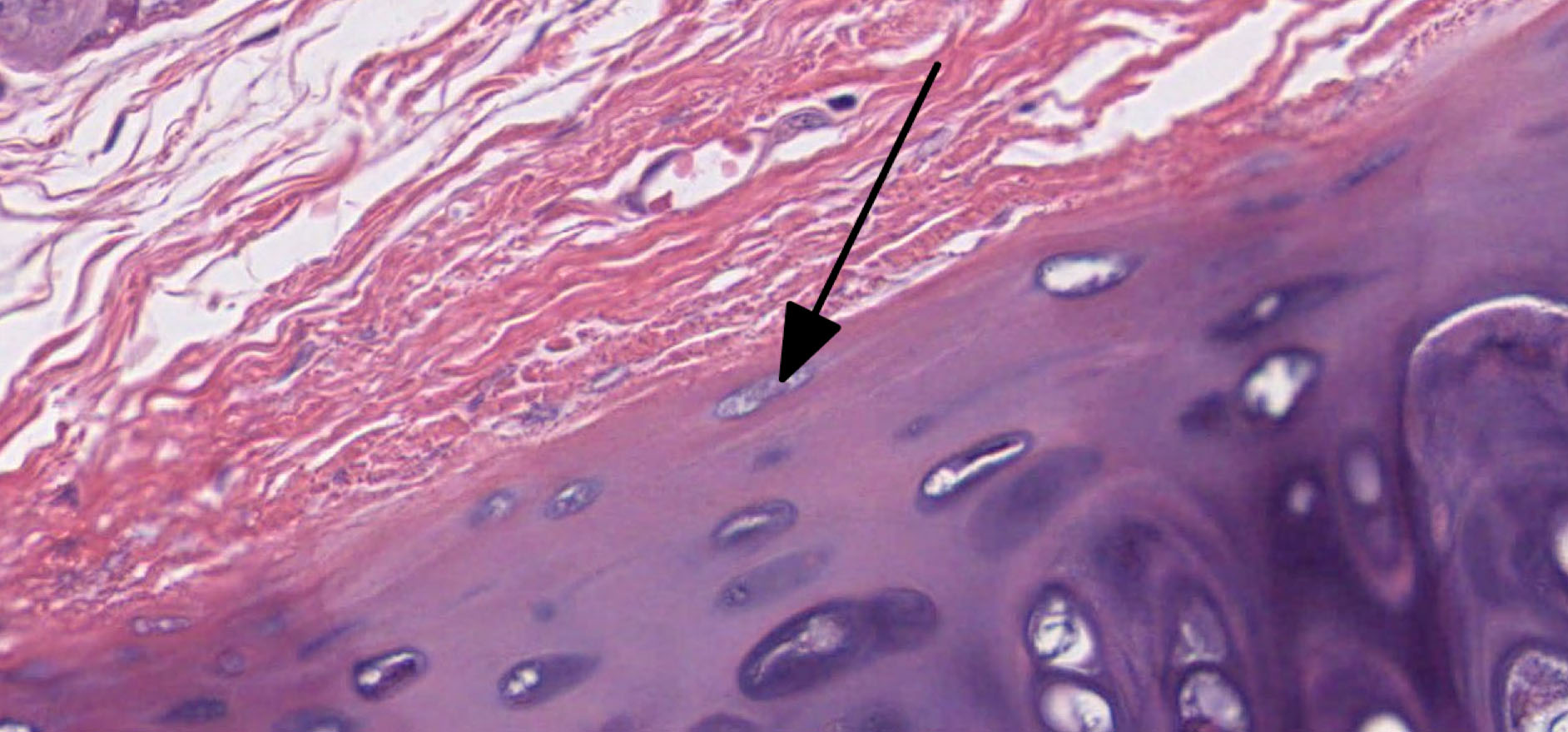
3. Identify the cell whose nucleus is marked by the black arrow.
- Chondrocyte
- Chondroblast
- Osteogenic progenitor cell
- Osteocyte
- Connective tissue fibroblast
Answer
Correct answer 2. A chondroblast in hyaline cartilage. It is OVOID and not yet surrounded by a lacuna. Therefore, it is a CHONDROBLAST. Osteogenic progenitors are located in the connective tissue perichondrium.
Mature Bone
- Be able to recognize compact and cancellous bone in conventional and ground sections and know the structural differences between the two types of bone.
- Be able to identify the components of adult bone and know their functions (e.g., periosteum, endosteum, osteons, canaliculi, lacunae, osteocytes, central/Haversian systems/canals, and Volkmann’s/perforating canals).
- Be able to recognize different bone cells at the light and EM levels and know their functions (e.g., active and inactive osteoblasts, osteocytes, osteoclasts).
- Know the major differences in matrix contents between cartilage and bone.
Slide 50 (fibula, monkey, decalcified, H&E) View Virtual Slide
Prior to sectioning and staining, this sample was soaked in a weak acid solution thus dissolving the mineralized component of the bone matrix but leaving behind all of the organic components (mostly type I collagen). Even though this section is distorted, you should be able to find osteons in various stages of development, lacunae, and canaliculi (to see canaliculi you will need to use your microscope and the glass slide from your collection --cut down the light by closing down the iris diaphragm to see them). The inner and outer circumferential lamellae slide 050 View Image can the bone shaft can also be seen in this section.
What distinguishes between compact and spongy bone?
Answer
Though it is easy to differentiate between compact and spongy bone at a gross level, at the microscopic level the main difference is the presence or absence of osteons. Grossly, compact bone has a dense appearance and is found, for example, on the outer surfaces of the long bones of the body. As the name implies, spongy bone is shaped like a sponge. The spaces within the sponge-shaped framework are filled with bone marrow. Compact bone, microscopically, is made of numerous osteons, whereas spongy bone is composed of sheets of lamellar bone and does not contain osteons.
Ground sections:
Cross sections:
Slide 051 Bone Ground section of compact cross View Virtual Slide
Slide 051XC Bone Ground section fibula cross View Virtual Slide
Slide 093B Bone Ground section of compact bone H&E cross section View Virtual Slide
Longitudinal sections:
Slide 093A Bone Ground section of compact longitudinal View Virtual Slide
Slide 051 Bone Ground section of compact longitudinal View Virtual Slide
Slide 051L-EX Bone Ground section of compact longitudinal View Virtual Slide
Slide 093C Bone Ground section of compact bone longitudinal View Virtual Slide
These "ground sections" were prepared by taking pieces of bone and grinding them with abrasives between two glass plates until they are thin enough to be semi-transparent. First, study cross sections (slides 51 and 93B). In these sections, the trapped air bends the light giving a dark image; the mineral and matrix generally transmit the light. You should be able to identify osteons and their subdivisions (as in slide 50), interstitial lamellae, Haversian/central canals and nutrient canals (Volkmann). Note that the latter canals penetrate osteons without causing new lamellae to be laid down around them. Note that slide 51XC is also an entire cross section of the fibula, so you should try to compare it against slide 50 discussed above.
Study the thinnest ground section (slide 93A) to identify lacunae and canaliculi. Now, look at the longitudinal sections (slides 51-20x, 51-40x, or 93C) of compact bone and try identifying the various structures mentioned above, especially Haversian/central and Volkmann's canals.
90 Osteocyte View Virtual EM Slide
The calcium crystals of the bone matrix were removed in this preparation by a decalcification process. Note how coarse the collagenous fibrils are and the difficulty in visualizing the periodicity of the fibrils (probably due to the process of mineralization).
93 Haversian canal View Virtual EM Slide
Note the "inactive" appearance of endosteal cells. The presence of a macrophage in the Haversian canal indicates the potential eroding function of the endosteal lining of the canal. Why are blood vessels so important in bone? (MatureBO2)
Click on a question to reveal the answer.
What distinguishes between compact and spongy bone?
Though it is easy to differentiate between compact and spongy bone at a gross level, at the microscopic level the main difference is the presence or absence of osteons. Grossly, compact bone has a dense appearance and is found, for example, on the outer surfaces of the long bones of the body. As the name implies, spongy bone is shaped like a sponge. The spaces within the sponge-shaped framework are filled with bone marrow. Compact bone, microscopically, is made of numerous osteons, whereas spongy bone is composed of sheets of lamellar bone and does not contain osteons.
Why are blood vessels important in bone?
Bone is a living tissue and, as such, needs a constant supply of nutrients. Without blood vessels, the bone would die.
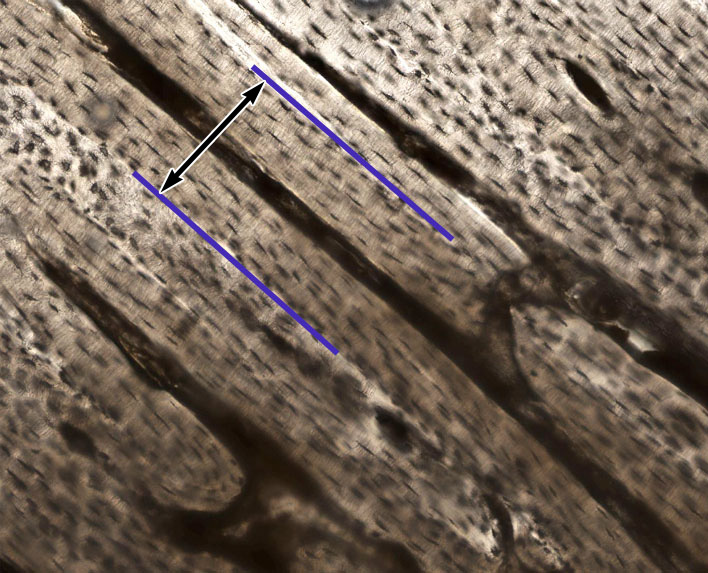
1. In this section of ground bone, identify the area indicated between the two purple lines.
- Outer circumferential lamellae
- Interstitial lamellae
- A Haversian system (osteon)
- A Volkmann's canal
- Inner circumferential lamellae
Answer
correct answer 3. A Haversian system (osteon) - this is a longitudinal section of compact bone showing LONGITUDINAL profiles of osteons consisting of concentric lamellae surrounding central Haversian canals (also in longitudinal profile). The canals that run PERPENDICULAR to the Haversian canals and it do NOT have any concentric lamellae organized around them are nutrient or Volkmann's canals.