Connective Tissue
- Describe the functions of cells commonly found in connective tissue and be able to identify them at the light and EM microscope level.
- Recognize interstitial (fibrillar) collagens and elastic fibers at the light and EM level.
- Distinguish between type I collagen, type III (reticular) collagens, and elastic fibers and recognized them in appropriately stained micrographs.
- Know about the physical characteristics of collagen and elastin and their functions in tissues where they occur in large quantities (e.g., type I collagen fibrils in dense connective tissue compared to more delicate type III collagen fibrils).
- Recognize different types of connective tissue (e.g., dense irregular, dense regular, loose, adipose) and know examples where they are found in the body.
- Recognize basement membranes (or basal lamina) in light micrograph and EM sections and know their functions.
NOTE: Please read the descriptions of the connective tissue stains BEFORE you do your lab work.
Slide 29 (small intestine, H&E) View Virtual Slide
Look at the connective tissue in the submucosa which is the lighter staining area View Image between the intestinal epithelium and the smooth muscle layer. In this area note the irregular, wavy collagen fibers arranged singly or in small groups. The collagen of fibrous supporting tissues, the dermis of the skin, tendon, ligaments and bone is type I collagen, which provides tensile strength. The background will be clear, reflecting a "ground substance"-rich connective tissue. Look for elongated nuclei, usually solitary, from which a modest amount of tapered cytoplasm extends from either one or both poles of the nucleus. These are fibroblasts View Image (as opposed to clusters of similar appearing elongate nuclei that are usually smooth muscle cells or Schwann cells in a nerve that you will learn to recognize soon). Note that the nucleoplasm of a fibroblast has a generally fine stippled (dot-like) chromatin pattern with occasional coarse chromatin clumps (heterochomatin) and one or two nucleoli. Look for more examples of fibroblasts and note that you rarely see much cytoplasm and that the nuclei of these cells can be quite condensed and hyperchromatic depending upon the plane of section or the metabolic state. You should be able to recognize a range of nuclear morphologies and be able to identify the cells as fibroblasts. Most of the rounded cells you may see in the submucosa are likely white blood cells (monocytes, macrophages, and occasional neutrophils) that have migrated out into the tissue.
Now look at the region immediately underneath the intestinal epithelium, which is called the lamina propria View Image . This region is also a loose, irregular connective tissue but can be so extensively infiltrated by white blood cells and plasma cells that the supporting fibers and ground substance are obscured. Neutrophils and macrophages are also present and both are discussed below.
A. Plasma Cells
Slide 29 (small intestine, H&E) View Virtual Slide
Slide 40 (trachea, H&E) View Virtual Slide
Look for plasma cells within the lamina propria of slide 29 View Image. They are round to oval shaped cells with a distinct cell boundary and a nucleus set to one side. Note the coarse chromatin clumps organzed as radial spokes in the round nuclei which is therefore often described as having a "clockface" or "wagon-wheel" appearance. You should note that the cytoplasm is quite basophilic (i.e. "base loving" so it binds hematoxylin and stains dark blue/purple), and, in well fixed tissue, the cytoplasm in many of the plasma cells is frequently granular (the rough endoplasmic reticulum, really) rather than smooth or even in appearance.
Find the Golgi complex, a pale or slightly eosinophilic (=eosin "loving", an area rich in membranes containing basic amino acids, syn. = acidophilic) region adjacent to the cell nucleus. The Golgi complex in these particular plasma cells is usually in the form of a fine crescent adjacent to the nucleus and it takes some practice to recognize.
Recall that the primary function of plasma cells is antibody secretion, so they are a prominent constituent of loose connective tissue wherever antigens may enter the body, such as the gastrointestinal, urogenital, and respiratory tracts. Plasma cells may also be foundwithin the connective tissue of many of the glands that secrete into these regions. An excellent example of this is slide 40 from the trachea (part of the respiratory tract). Look at the areas outlined in the orientation diagram of the trachea and locate the loose, cellular connective tissue within the glands (the "glands" are coiled tubes of columnar epithelial cells; some the epithelial cells are tall and eosinophilic, whereas others are shorter and more basophilic). In addition to some fibroblasts and a few delicate collagen fibers, you should see quite a few plasma cells View Image amongst the epithelial tubes
Slide 40 is also a very good specimen to examine the pseudostratified, ciliated columnar epithelium of the trachea. Note also that thebasement membrane underlying this particular epithelium is especially prominent. Type IV collagen, which does not form fibrils, but rather a fine meshwork, is present in all basement membranes. The basal lamina is anchored to the underlying connective tissue by fine fibrils oftype VII collagen (you obviously can't tell this looking at it in the light microscope, but you should recall this from lecture).
B. Neutrophils
Slide 29 (small intestine, H&E) View Virtual Slide
Look in the lamina propria amongst the plasma cells and you will find neutrophils that have emigrated from the bloodstream into the tissue space as part of the immune response. Neutrophils can be identified by their granular cytoplasm and their multilobular, condensed nuclei. Because of their nuclear morphology, they are frequently also called “polymorphonuclear leukocytes” (aka "PMNs" or “polys”). Neutrophils generally enter tissues in large numbers only in response to a disease stimulus. However, as seen in this slide, it is quite normal to find them in tissues such as the gut where foreign substances frequently invoke an inflammatory response. You will study neutrophils in much greater detail in other sequences and in your histopathology course, but it is useful for now to at least be able to recognize them in various tissues and organs.
C. Macrophages
Slide 26 (lymph node, H&E) View Virtual Slide
With low power, locate the medulla (the interior) of the lymph node. Look for a region characterized by interlacing cords of cells. Macrophages are the biggest, rounded cells that are floating free in the spaces between the cords of cells. Many of the free cells in these medullary sinuses cannot be identified; however, the large rounded cells, with eccentrically placed, vesicular nuclei are the ones you should try to find.
Many of these macrophages contain phagocytosed red blood cells or the brownish breakdown pigment, hemosiderin (which is the result of lysosomal action on the ingested red blood cells.). Be sure you can identify a macrophage and not just a bunch of cells superimposed upon one another. Macrophages can be seen also in the subcapsular sinus (the lighter staining area just under the capsule at the periphery of the lymph node).
The "mononuclear phagocyte system" (also called the "reticuloendothelial system" for historic reasons) consists of free and fixed macrophages throughout the body. These cells are important in removing all kinds of debris from the body as well as playing a major role in the immune response.
D. Fat Cells
Slide 152 (pharynx, H&E) View Virtual Slide
Slide 30 (mesentery, H&E) View Virtual Slide
Slide H2 (fetal thorax, H&E) View Virtual Slide (virtual slide courtesy of Western University)
Slide 152 is a section from the pharynx. Locate the large clear circles View Image in the connective tissue that sits beneath the epithelium. These are cells (or adipocytes). In white or unilocular adipose tissue, lipids are stored as a single, non-membrane bound droplet in these cells. A fatty tissue called brown or multilocular fat, produced during fetal development, has adipocytes that contain multiple fat droplets. Brown fat is important for thermoregulation in newborns and hibernating mammals. In humans, brown fat is widely distributed throughout the body in the first decade of life, but it then disappears except for regions around the kidney, suprarenal glands, aorta, neck and mediastinum. None of our slides of adult tissue shows any brown fat, however this rather unique tissue can be seen in slide H2 View Image, which is from a developing fetus.
Look for adipose tissue in Slide 30 which is taken from abdominal mesentery (the connective tissue that suspends the viscera within the abdominal cavity). Some of the individual fat cells are often broken during tissue preparation, but the overall impression of what the tissue looks like is the important point.
E. Mast Cells
Slide 160 (stomach, PAS & Azure II) View Virtual Slide
Mast cells can only be definitively recognized with special stains such as Azure II and toluoidine blue that identify the heparin storage granules (Azure metachromatically stains the heparin purple). Mast cells are most abundant in the connective tissue associated with the lining of the digestive and respiratory systems, and your collection just so happens to contain a tissue section from the stomach that has been stained with PAS and Azure II. As you look at this section, you will see a very obvious layer of mucous epithelial cells (PAS also reacts with the carbohydrate-rich mucin). However, to see the mast cells, you will need to look deeper in the submucosa where you should find small, ovoid cells amongst the collagen fibers with spherical, eccentric nuclei and intensely basophilic (dark purple to black) granulesView Image. The granules are often so dark that they obscure the nucleus.
Slide 27 (lymph node, H&E) View Virtual Slide
Slide 28 (lymph node, silver stain) View Virtual Slide
The fine collagenous network that provides support in the bone marrow, lymphatic organs, around individual smooth muscle cells, and beneath most epithelia is composed mainly of Type III collagen. The collagen has an associated carbohydrate moiety (uncharacterized) that can reduce Ag+ to metallic Ag revealing a network (reticulum) of fine, black fibrils. These are termed reticular (or rarely, argyrophilic= "silver loving") fibers. On slide 27 look at the accumulations of darkly stained cells (lymphocytes in a lymph node). Note at high power that fibrils or fibers of any type cannot be readily observed. Now with slide 28 (make sure your slide is stained with silver; it should say “Ag” on the label!), note how a network of fine black fibrils is present in this same tissue following silver staining. These are reticular fibers, found in skin, muscle and blood vessels. The reticular fibers provide physical support for all the cells present in tissues subject to stretching. You are not responsible for recognizing reticular fibers unless a silver stain is used.
Please remember that virtually all cells (except for those in the brain and spinal cord) are provided with some degree of support by collagen (reticular fibers) even though that may not be apparent with H&E staining. (Masson Trichrome and silver staining are frequently used in pathology to determine if connective tissue has proliferated--a sign of damage and attempted repair--in the liver, kidney and lung.)
A. DENSE IRREGULAR CONNECTIVE TISSUE
Slide 33 (skin, Verhoeff stain) View Virtual Slide
Slide 250-1 (vagina, H&E) View Virtual Slide
Slide 250-2 (vagina, trichrome) View Virtual Slide
The area beneath the stratified squamous epithelium shown in slide 33 is the dermis, which is composed of dense irregular connective tissue. In this section, the fibers clearly predominate. This slide has been stained with iron hematoxylin and eosin so you can see collagen fibers (orange) as well as elastic fibers (purple/black) in the dermis View Image. Note how the diameter of the fibers varies with location. In the region immediately beneath the epidermis you can see how the elastic fibers are interconnected forming an elaborate, delicate net of fibers View Image amongst thin strands of collagen. However, deeper in the dermis, the collagen and elastic fibers are much thicker.
Slide 250 which you used to look at stratified squamous non-keratinizing epithelium is also useful for the study of connective tissue (we will also use this slide to study smooth muscle and peripheral ganglia). Be sure you look at both the H&E and Masson trichrome-stained slides as they provide an excellent opportunity to see how collagen stains in connective tissue when either stain is applied. When we study smooth muscle and peripheral nerve tissue we will come back to this slide to try and distinguish between collagen fibers and fascicles of smooth muscle and/or nerve fibers and ganglia.
NOTE: Slide 250 illustrates a point about the limits of classification schemes. Even though we try to set up rigid categories (e.g. "loose" versus "dense" connective tissue), sometimes it is not always possible to classify connective tissue in a given section; it may be a little loose, a little dense, a little fatty, etc. In these particular instances, don't worry so much about trying to exactly classify the tissue per se, but at least try to identify the cellular and extracelluar components that you can (also bear in mind that you can't always definitely identify every cell) and think how its overall appearance reflects its function.
B. DENSE REGULAR CONNECTIVE TISSUE
1. Collagenous
Slide 106 (plantar skin and tendon, H&E) View Virtual Slide
Slide 112 (plantar skin and tendon, H&E) View Virtual Slide
Slide 106 and 112 have bits of well preserved flexor tendon at the top of the section (the tissue at the very top of slide 112 is actually skeletal muscle -which you'll study in the next lab; the tendon is just below it). Note the regular orientation of the collagen fibers (there's a bit a "waviness" but you should get the idea). You should also observe that there aren't a lot of cells, a characteristic of "dense" connective tissue. The very small cracks between the fibers are just artifacts of shrinkage that occured during tissue preparation. Of course, there are some places where there are breaks in the dense regular connective tissue of the tendon containing loose connective tissue associated with nerves and blood vessels or the occasional bit of adipose tissue.
2. Elastic tissue
slide 36 (Aorta, aldehyde fuchsin) View Virtual Slide
slide 88 (Aorta, H&E) View Virtual Slide
These slides are examples of regularly arranged sheets (lamellae) of elastin. Slide 36 is stained with aldehyde fuchsin and Masson trichrome (Aldehyde Fuchsin, Fe. Hem. & Mass.), so the elastic lamellae are purple. Slide 88 is stained with H&E where the concentric rings of elastic lamellae are intensely stained with eosin giving a glassy red appearance View Image (one of the few places where elastin is easy to recognize in H&E sections).
Two other locations where elastic fibers can be readily seen in H&E sections are in the lamina propria of the pharynx (slide 152 View Image ) and the trachea (slide 40 View Image ). Unlike the tissue of the aorta which would be classified as "regular," these tissues are obviously irregular but they're mentioned here for the purpose of illustrating how aggregates of elastic fibers appear in H&E-stained sections. Just as in the H&E-stained aorta, the elastic fibers in the pharynx and trachea are glassy and orange-red --they appear as stippled dots because they’ve been cut in cross section.
26 Connective Tissue - Dense Irregular View Virtual EM Slide
Dense Connective Tissue. Note the alternating layers of fibroblasts and collagenous fiber bundles. Make sure you can see the difference between cross sectioned and longitudinally sectioned collagenous fibrils. In dense connective tissue, which type of cell is most common? (CT7)
18 Loose Connective Tissue - Lamina propria of tracheal mucosa View Virtual EM Slide
Loose Connective Tissue. In this micrograph of loose connective tissue of the tracheal mucosa numerous (labeled) cells of the connective tissue are present. Note the relative size of the different cell types, their shapes, amount of rough ER and variously sized granules and inclusions. Then use your text and atlas to review the diagnostic features of each connective tissue cell present in the micrograph. Note the paucity of collagen fibrils. What was present in the "empty" looking intercellular space? (CT10)
27 Elastic Connective Tissue - Junction of Media and Adventilia of artery View Virtual EM Slide
Observe the branching nature of the elastic fiber and the "mantle" of elastic microfibrils. The cross banding of the collagenous fibrils is easily observed.
28 Collagen and Elastin - Cross section of Chorda Tendinea View Virtual EM Slide
Observe the mixture of collagen and elastic fibers in this cross section of chorda tendinea. Although collagen fibers mostly fill the view, there are numerous elastic fibers, which provide the elasticity essential for the function of the tissue.
29 Tendon - Longitudinal section View Virtual EM Slide
Note the uniform distribution of regularly arranged collagen fibers (type I).
25 Connective Tissue - Fibroblast View Virtual EM Slide
Observe the large amount of rough endoplasmic reticulum (ER) in these cells. Is this an indication of an active or inactive cell? (CT9) Test your ability to identify different organelles at this magnification!
20 Mast cell - Human View Virtual EM Slide
Mast cells contain a mixture of granule types reflective of the variety of substances they secrete. Histamine and heparin are found in the more "regular" looking granules (evenly dark and round). Other secretory products include leukotrienes and other phospholipid derivatives, which are made from the sheets of membranes arranged as lamella, whorls, or even scroll-like bodies within the more irregular appearing granules. What are the secretory products of the mast cell? (CT11)
63 Macrophage View Virtual EM Slide
Tissue macrophages can be found in many different organs. As they have a phagocytic function, removing pathogens and cell debris, macrophages usually contain abundant primary and secondary lysosomes.
21 Plasma cell View Virtual EM Slide
This electron micrograph shows a typical secretory cell, a plasma cell, which secretes immunoglobulin protein. Many of the major types of cellular organelles are visible in this image. In the nucleus, areas of euchromatin and heterochromatin can easily be identified. Use these micrographs to review the structure of organelles. Be sure you recognise favourable sections of the nucleas, mitochondria, and rough ER.
23 Fat Cells - Mature View Virtual EM Slide
This electron micrograph depicts mature fat cells. You can see one large lipid droplet in the cytoplasm of each cell. The nuclei of many cells are not included in the field of view. Brown fat cells would have several small lipid droplets all of which would be roughly the same size. Remember that each fat cell is enclosed by a thin basal lamina (Unfortunately, in these examples you can’t see the basal lamina). Where are the nuclei of the fat cells? (CT8)
Click on a question to reveal the answer.
What type of epithelium lines the luminal surface of the intestine?
The luminal surface of the intestine is made up of a simple columnar epithelium.
Why is rough endoplasmic reticulum basophilic?
The ribosomes attached to rough ER are associated with both ribosomal and messenger RNA - these nucleic acids carry a net negative charge and bind basic dyes (which are positively charged).
What type of lining epithelium is present in the pharynx?
Stratified squamous non-keratinizing epithelium lines the pharynx.
Can you see a nucleus in each fat cell?
No, because not all nuclei are on the plane of section.
What do mast cells do?
Mast cells are actively involved in a host's immune response and produce many substances, some of which are heparin and histamine. The degranulation of these cells is responsible for triggering type I, immediate hypersensitivity reactions. Type I reactions, also called anaphylactic reactions, are something you will learn about while studying the immune system later on, but for now, here is a quick explanation. IgE is an antibody, produced by plasma cells, that has a high affinity for mast cells and basophils. The antibody binds mast cells and waits for a second exposure to whatever it happens to be responsive to (an allergen). When the IgE binds an appropriate molecule, it will trigger degranulation of the mast cell and the vasodilation, congestion, bronchiolar constriction, wheezing, etc. associated with allergies and other type I reactions
Why do cells actively secreting proteins exhibit basophilic cytoplasm?
Protein secreting cells have a basophilic cytoplasm because they are full of rough ER, which stains with hematoxylin, a basic dye.
In dense connective tissue, which type of cell is most common?
Dense connective tissue is full of fibroblasts.
Where are the nuclei of fat cells?
Fat cell nuclei are on the periphery of the cell and may or may not be in the plane of section.
Is rough ER an indication of an active or an inactive cell?
Large amounts of rough ER indicate that the cell is active and is producing large amounts of proteins.
What was present in the "empty" looking intercellular space?
The empty space within connective tissue is ground substance.
What are the secretory products of the mast cell?
Heparin and histamine are just some of the contents of mast cell granules.
1. Which statement about the cells marked by the black arrows is true?
View Image

- They produce collagen.
- They are derived from mesenchymal progenitor cells.
- They secrete antibodies.
- They release histamine during allergic reactions.
- They phagocytose cell debris and/or foreign material.
Answer
Correct answer 5. They phagocytose cell debris and/or foreign material. The cells indicated are macrophages, which are derived from hematopoietic progenitors and function primarily in the phagocytosis of cells and debris and antigen processing and presentation.
2. Identify the tissue depicted in the below micrograph.
View Image
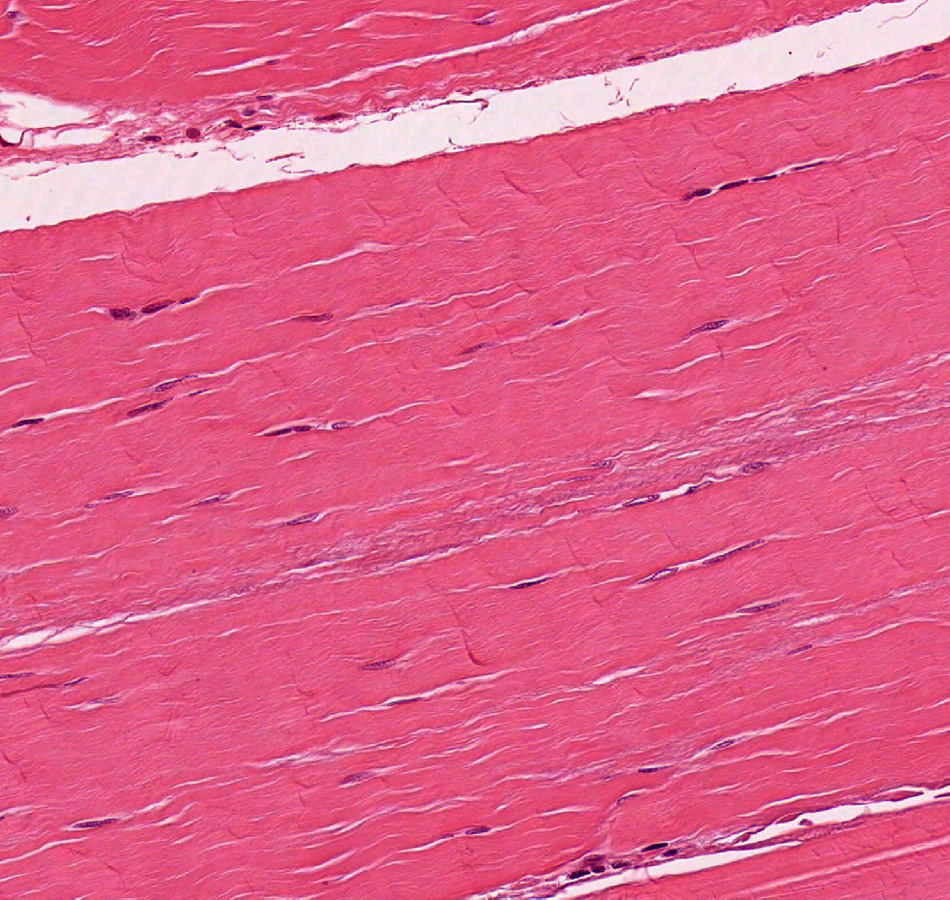
- Stratified squamous keratinized epithelium
- Stratified squamous non-keratinized epithelium
- Dense regular connective tissue
- Dense irregular connective tissue
- Loose connective tissue
Answer
Correct answer 3. Dense regular connective tissue - the tissue shown has a dense, regular arrangement of collagen fibers; the cells present are fibroblasts NOT squamous epithelial cells.
3. Identify the structure that is enclosed by the brackets in this electron micrograph.
View Image
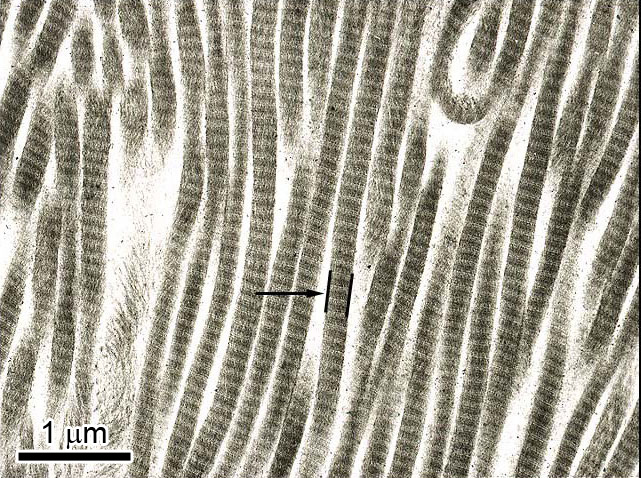
- Pro-alpha collagen chain
- Procollagen triple helix
- Tropocollagen triple helix
- Collagen fibril
- Collagen fiber
Answer
Correct answer 4. A collagen fibril -the brackets enclose a single collagen FIBRIL, which is made of 1000s of tropocollagen units attached in a head-to-tail arrangement. Multiple fibrils are bundled together to form a FIBER (which is what you can see in the light microscope). Finally, recall that PROcollagen is INTRAcellular and doesn't aggregate into fibrils as shown here until secreted.
4. This tissue section stained with aldehyde fuchsin and eosin. Identify the correct statement about the structure that is indicated by the black arrow.
View Image
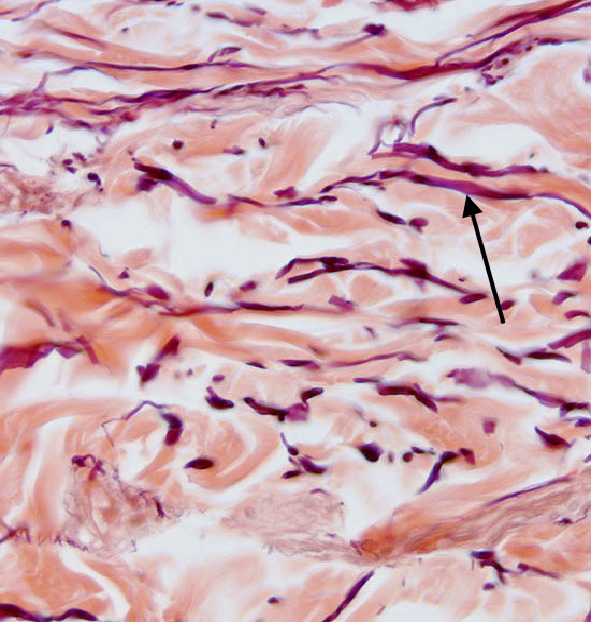
- It is comprised primarily of type I collagen.
- It is comprised primarily of type II collagen.
- It is secreted by plasma cells.
- It is significantly weaker in individuals with Marfan syndrome.
- It is significantly weaker in individuals with type IV Ehlers-Danlos syndrome.
Answer
Correct answer 4. It is significantly weaker in individuals with Marfan syndrome. The structure indicated is an elastic fiber, which stains purple/black with aldehyde fuchsin and would be significantly weaker in individuals with Marfan syndrome.
