Salivary Glands
1. Identify parotid, submandibular, and sublingual salivary glands on the basis of their histological appearance and by the type of secretion each gland produces.
2. Identify the three types of ducts (intralobular, intercalated, striated, interlobular) in salivary glands at the light microscope and the EM level and correlate their structural features with functional aspects of these ducts.
3. Know the localization of myoepithelial cells and nerves in relation to the acinar cells, and their role in secretory functions.
We will study three major salivary glands; the parotid, submandibular, and sublingual glands. These glands are divided into numerouslobules which contain the secretory units, which are called acini. Each secretory unit consists of acinar (secretory) cells and branching ducts. Ducts within lobules (intralobular ducts) connect with larger interlobular ducts which are found in the connective tissue between lobules.
Slide 184 Submandibular gland H&E View Virtual Slide
Tasks:
- find serous and mucous acini
- find serous demilunes
- find myoepithelial cells
Unlike the parotid gland, the submandibular and sublingual glands possess both mucous and serous secretory cells. Mucous cells have a pale-staining, bubbly cytoplasm and nuclei that appear to be pushed against the basal cell membrane. In contrast, the cytoplasm of serous cells contain distinctly eosinophilic zymogen granules and their nuclei are spherical in appearance. Compare the appearance of mucous and serous secretory cells and be sure you can tell the difference. The secretory cells are organized into secretory units or acini, and they are classified according to the cell types they contain:
- serous acini - contain only serous cells and are generally spherical
- mucous acini - contain only mucous cells and are generally tubular
- mixed (or sero-mucous) acini -contain a mixture of serous and mucous cells. In routinely-prepared tissue sections, the mucous cells swell and "push" the serous cells into a peripheral cap known as a serous demilune (demilune = "half-moon")
Slide 180-1 Parotid gland H&E View Virtual Slide
Slide 180-2 Parotid gland H&E View Virtual Slide
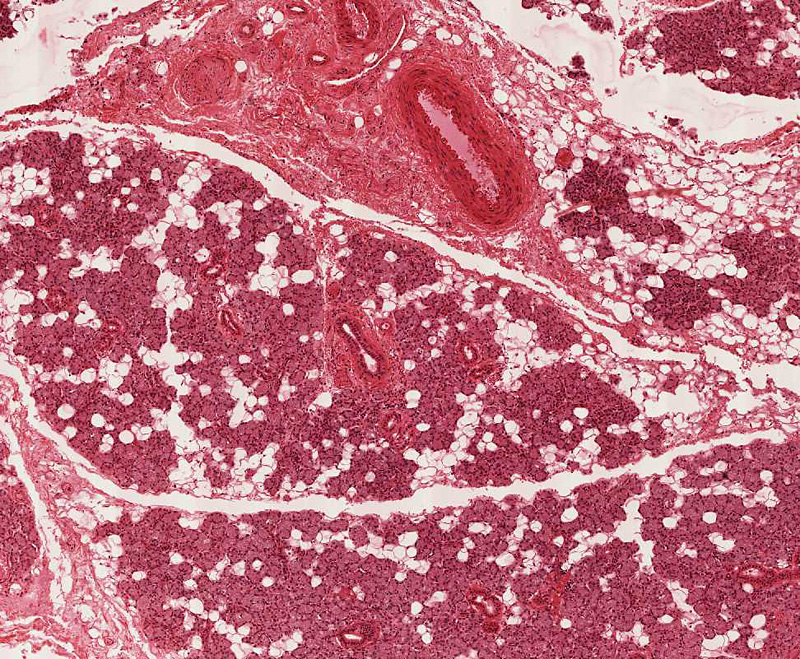
Using the low power objective, observe the abundance of fat in this gland: the amount of fat increases with age. Note that the parenchymal(secretory) tissue is divided into many lobules by the stromal (supportive) connective tissue. In this connective tissue stroma, notice the presence of blood vessels, nerves and large excretory ducts (interlobular). These interlobular ducts slide 180-2 View Image are lined by a pseudostratified columnar epithelium. Find a well defined lobule slide 180-2 View Image and observe the secretory acinar cells and ducts. You will note that these acinar cells are fairly uniform in size, structure and staining, because they all produce proteinaceous (serous) secretion. The secretory granules are not well preserved by routine methods of light microscopic fixation and are not recognizable in this slide.
With each lobule are intralobular ducts which are lined by a simple columnar epithelium of varying heights (becoming progressively taller toward the point at which the intraclobular ducts empty into interlobular ducts). The intralobular ducts are, in turn, further subdivided into striated and intercalated portions. Since the striated portions are much longer, you will see many more of them and we'll consider them first. Select a transverse section of a striated duct slide 180-2 View Image and observe the fine striations at the basal portions of the lining cells.
What are the "striations" of striated ducts?
Answer
The striations, noted with the light microscope, are due to vertical alignment of numerous long mitochondria in narrow compartments formed by deep invaginations (infoldings) of the plasma membrane at the cell base. These cytological specializations are for efficient active transport of water and ions to modify the primary secretion of the acini during its passage through this portion of the duct to a hypotonic solution containing high concentrations of bicarbonate.
The slender, intercalated ducts slide 180-2 View Image connect the secretory acini and striated ducts, but the intercalated ducts in this gland are much shorter than those in the pancreas (which we will cover in another session), so they are not as easy to spot.
Submandibular Gland:
Slide 183-1 Submandibular gland H&E View Virtual Slide
Slide 183-2 Submandibular gland (homo) 20X, mucicarmine stain [stains mucus red] View Virtual Slide
Slide 184 Submandibular gland H&E View Virtual Slide
Sublingual Gland:
Slide 185-1 Sublingual Gland 40X H&E View Virtual Slide
Slide 185-2 Sublingual Gland 40X H&E View Virtual Slide
Slide 185A Sublingual gland 20X mucicarmine and H&E stain [stains mucus red] View Virtual Slide
Unlike the parotid gland, the submandibular and sublingual glands possess both mucous and serous secretory cells. Slides 183-2 (submandibular) and 185A (sublingual) are stained with mucicarmine, which specifically stains mucus red. Survey the two alternate slides to compare the relative proportions of mucous acini in these two glands. After this, go back to the H&E-stained slides to study the histology of mucous and serous secretory acini.
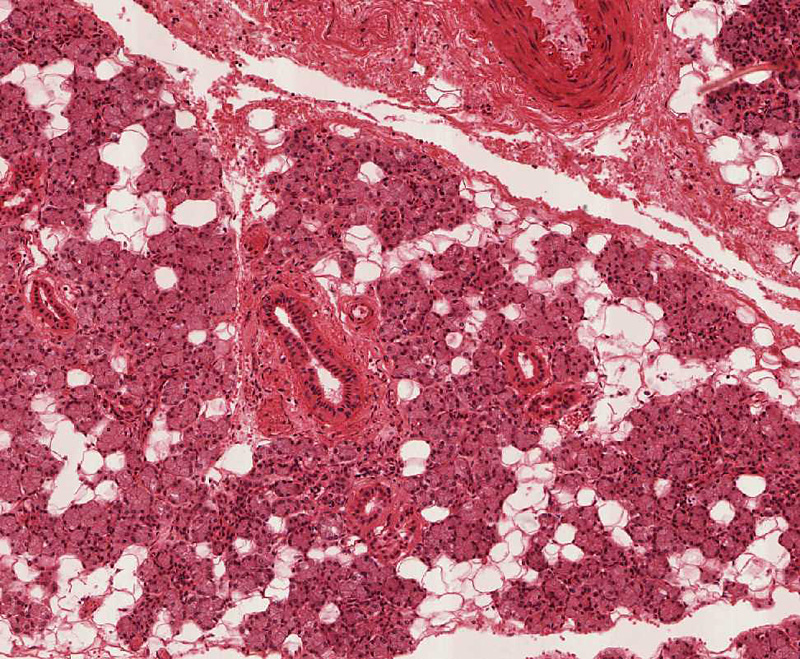
In slide 183 and 184 of the submandibular gland, mucous secretory acini are those that stain lightly. Compare the appearance of mucous and serous secretory cells. The serous cells possess granular cytoplasm and nuclei which are spherical and vesicular in appearance. The mucous cells have pale staining cytoplasm and nuclei which appear to be pushed against the basal cell membrane. Now, observe the blind end of a mucous acinus and note the serous demilune cells View Image that cap this region of the secretory acinus. These demilune cells also have brightly staining granules in their cytoplasm. As an aside, the serous and mucous cells are actually adjacent to each other in vivo, and the formation of these demilunes is actually a fixation artifact (mucous cells swell with traditional fixation techniques and “squeeze out” the serous cells). Even so, the characteristic appearance of demilunes is nonetheless a useful diagnostic for identifying sero-mucous glands. Switch to a lower power and observe the distribution of ducts. Note the presence of large ducts in the connective tissue septae separating the lobules. These are interlobular or excretory ducts View Image and their epithelium appears to be stratified. The intralobular ducts within the lobules are smaller and similar in appearance to those of the parotid gland (i.e. they are striated ducts). The intercalated ducts in the submandibular and sublingual glands are very short and therefore NOT encountered often in sections.
Now examine slide 185-1 and 185-2, the sublingual gland, and note the greater prominence of mucous acini and fewer numbers of intralobular ducts than in the submandibular gland. Some lobules in slide 185-1 and 185-2 reveal almost all ducts with a few remaining secretory cells. This represents a pathological transformation of secretory acini to duct-like structures.
187 Glands - Lingual Mucous Glands Mucous Acinus of a Lingual Salivary Gland View Virtual EM Slide
Note the accumulation of mucin-containing secretory vesicles next to the lumen of the secretory acinus depicted in this electron micrograph.
Click on a question to reveal the answer.
What are the "striations" of striated ducts?
The striations, noted with the light microscope, are due to vertical alignment of numerous long mitochondria in narrow compartments formed by deep invaginations (infoldings) of the plasma membrane at the cell base. These cytological specializations are for efficient active transport of water and ions to modify the primary secretion of the acini during its passage through this portion of the duct to a hypotonic solution containing high concentrations of bicarbonate.
Mammary Gland
1. Identify the histological components of the mammary gland, including structures associated with the nipple and the areola, the overall organization into lobes and lobules, as well as secretory alveoli (acini), lactiferous ducts/sinuses, and the intralobular and interlobular connective tissue.
2. Identify and describe the histological differences between the mammary gland in adult females prior to pregnancy (inactive), during pregnancy, and during lactation (active).
3. Know the cellular mechanisms involved in the formation and release of milk.
Slide 265 Nipple, areola H&E View Virtual Slide
The 16-20 lactiferous ducts slide 265 Nipple, areola H&E View Image, one from each lobe, open at the summit of the nipple. These ducts are lined by stratified squamous epithelium near the opening and the lumens are frequently filled with desquamated cells. Deeper in the connective tissue, the ducts acquire a stratified columnar appearance that is really a cuboidal duct cell sitting on a myoepithelial cell as in the sweat gland.
Sebaceous glands slide 265 View Image are present to a variable extent, especially in the areola. Note that the dense irregular connective tissue of the dermis is interrupted by numerous fascicles of smooth muscle slide 265 View Image that insert into the dermal connective tissue (much like arrector pili muscles). These muscle bundles are responsible for erection of the nipples. Occasional nerves are also present in the dermis.
Slide 259 Mammary gland inactive nulliparous H&E View Virtual Slide
Slide 258 Mammary gland active, pregnant H&E View Virtual Slide
Slide 261 Mammary gland active lactating H&E View Virtual Slide
Like the other tissues in the female reproductive system, alterations in circulating hormone levels result in histologically demonstrable changes in the mammary gland. Compare the examples of an inactive and active glands, noting the differences in the amount of glandular tissues. In slide 259 (inactive gland) note the dense irrengular interlobular connective tissue found between quiescent glandular lobulesthat consist of only a few clusters of small ducts surrounded by a mass of less dense intralobular connective tissue. Many ducts appear to be composed of 2 layers of cuboidal epithelium. The inner layer are the actual ductal epithelial cells whereas the outer layer of cells is, in fact, a layer of myoepithelial cells.
In slide 258 (active gland), you can see that the amount of the glandular tissues has increased, while that of the connective tissue has decreased. This increase involves the numbers of both the epithelial cells and myoepithelial cells. The proliferation of these cells lead to the formation of secretory alveoli. Note also the increased cellularity (especially, the plasma cells) of the intralobular connective tissue. This tissue was probably taken from an individual before the last trimester. When compared with the inactive mammary gland, you can see that the intralobular ducts have proliferated to form additional secretory regions. Both the epithelial cells and myoepithelial cells increase in number. Alveoli slide 261 View Image have formed, their epithelial cells have large, clear areas of apical cytoplasm, a region occupied by glycogen and lipid. Note the increased cellularity of the intralobular connective tissue. Note also that not all lobules within the gland have proliferated to the same degree. In many sections, portions of a large excretory, lactiferous duct slide 261 View Image are present. The epithelial lining is again two layered, the bottom layer being principally myoepithelium. Compare the morphology of the inactive and active gland. Observe the intralobular connective tissue and note the abundance of plasma cells slide 261 intralobular connective tissue and note the abundance of plasma cells View Image. These plasma cells are the source of secretory IgA.
290 Mammary gland View Virtual EM Slide
Observe the process of true apocrine secretion. Lipid granules are released covered with a small amount of mammary gland cell cytoplasm, as well as the cell membrane. On the other hand, the protein components are released by the usual mechanism of exocytosis.
Click on a question to reveal the answer.
What is the difference between intralobular and interlobular connective tissue?
Intralobular connective tissue (the connective tissue around the ducts of each lobule) is a looser, more vascular and cellular connective tissue. The cellularity comes not only from fibroblasts, but also from an abundant number of plasma cells that produce the IgA that is secreted into the milk. Interlobular (between lobules) connective tissue, on the other hand, is dense and collagenous and contains fewer cells.