Oral Cavity
- Know the location and histological features of different types of oral mucosa (lining, masticatory, specialized).
- Know the histology of the tongue including taste buds and different types of papillae.
- Know the histology of the adult tooth and name the cells responsible for the production of enamel, dentin, and cementum.
- Describe how a tooth is anchored in alveolar bone.
- Know the structure of the epithelial attachment and understand its significance in protecting the periodontal space.
The oral cavity is lined by a mucous membrane (the oral mucosa) consisting of a stratified squamous epithelium, which may or may not be keratinized, and an underlying connective tissue layer, the lamina propria. The surface is kept moist with mucus produced by the major and numerous minor salivary glands. The oral mucosa is well supplied with nerve endings and, on the dorsal surface of the tongue, special sensory endings for taste. The submucosa underlying the lamina propria of the oral cavity is variable. At times the lamina propria and submucosa are substantively so similar that they merge imperceptibly. In your slides, the submucosa will be distinguished from the lamina propria only by the presence of minor salivary glands in a loose textured tissue, and we do not ask you to recognize this distinction microscopically.
1. Lining Mucosa
Slide 114R (lip, human, H&E) View Virtual Slide
Slide 114 triC (lip, human, trichrome) View Virtual Slide
Slide 114M (lip, monkey, H&E) View Virtual Slide
A stratified squamous non-keratinized epithelium lines the oral surface of the lips, cheeks, floor of mouth, and covers the ventral surface of the tongue In slide 114 (human) and 114M (monkey) of the lip, note that skin (stratified, keratinized squamous epithelium with hair follicles) covers the external surface View Image, skeletal muscle (orbicularis oris muscle) forms the core View Image, and a mucosal epithelium(stratified, non-keratinizing squamous epithelium) covers the internal surface View Image. A lamina propria underlies the mucosa and small salivary glands (labial salivary glands) View Image are present in the submucosa. Note the transition zone between the keratinized epithelium of the skin and the nonkeratinized epithelium of the mucosa. This transition zone is called the vermillion zone (present only in humans) View Image. In the transition zone, long connective tissue papillae extend deep into the epithelium. Capillaries are carried close to the surface in these papillae. Because the epithelium is very thin in this region, the lips appear red (this arrangement may or may not be apparent in your glass slides). Salivary glands are lacking in the vermillion zone, therefore, the lips must be continuously moistened (by the tongue) to prevent drying out.
2. Masticatory Mucosa
Slide 115 (fetal palate, H&E) View Virtual Slide
Slide 115 (fetal palate, trichrome) View Virtual Slide
A stratified squamous keratinized epithelium is found on surfaces subject to the abrasion that occurs with mastication, e.g., the roof of the mouth (palate) and gums (gingiva). Slide 115, which you used to study bone and the respiratory system, is a longitudinal section through the palate and includes the lip, gingiva, hard palate, and a portion of the soft palate [orientation]. This tissue is from a term fetus (with unerrupted teeth) and the epithelium over the hard palate is not yet fully differentiated (i.e. not fully keratinized). The slide is, however, a good overall orientation to the histology of the hard and soft palate. In the adult the epithelium of the hard palate is keratinized. Identify respiratory epithelium, bone (hard palate), forming tooth View Image, and skeletal muscle in the lip View Image and the soft palate View Image. Some slides show mucous salivary glands View Image in the submucosa.
3. Specialized Mucosa
Slide 116 40x (tongue, H&E) View Virtual Slide
Slide 117 20x (tongue, H&E) View Virtual Slide
Slide 117 40x (tongue, H&E) View Virtual Slide
Slide 117N 40x (tongue, rabbit, H&E) View Virtual Slide
The dorsal surface and lateral borders of the tongue are covered by a mucous membrane that contains nerve endings for general sensory reception and taste perception. In slide 116, the dorsal surface of the tongue is covered with tiny projections called papillae View Image, which are lacking on the ventral surface. The body of the tongue is composed of interlacing bundles of skeletal muscle View Image that cross one another at right angles. The dense lamina propria of the mucosa is continuous with the connective tissue of the muscle, tightly binding the mucous membrane to the muscle. Some glass slides in our collection show mucous glands in the submucosa, which are found only on the ventral side of the tongue. These glands are not present in the digital slides, but their ducts may be seen View Image.
In slide 116 there are two types of papillae on the tongue. Locate the numerous filiform papillae View Image, that appear as conical structures with a core of lamina propria covered by a keratinized epithelium. Fungiform papillae View Image are scattered among the filiform papillae. They have expanded smooth round tops and narrower bases. In young children, the fungiform papillae can be seen with the naked eye as red spots on the dorsum of the tongue (because the non-keratinized epithelium is relatively translucent). These papillae are less readily observed in adults, because of slight keratinization of the epithelium.
Slide 117 and especially slide 117N contain examples of circumvallate papillae View Image. These are large circular papillae surrounded by a deep trench. The covering epithelium is non-keratinized. Taste buds View Image, the chemoreceptors for the sense of taste, are located on the lateral borders. Each taste bud contains about 50 spindle shaped cells that are classically described based on their appearance as “light” (receptor) cells, “dark” (supporting) cells, and “basal” (stem) cells, although these distinctions are difficult to see in your slides so we do not require you to identify the cell types. Non-myelinated nerves from cranial nerves VII, IX, or X (depending on the location of the taste bud) synapse with the receptor and, to some extent, supporting cells of the taste bud. Some slides show serous glands (of von Ebner) View Image in the lamina propria and interspersed between the bundles of muscle beneath the papillae. These glands drain into the base of the trench around the circumvallate papillae.
Slide 122 40x (tooth, monkey, H&E) View Virtual Slide
Slide 122 20x (tooth, monkey, trichrome) View Virtual Slide
Slide 122PAS 20x (tooth, monkey, PAS) View Virtual Slide
Slide 123 40x (tooth, pig, H&E) View Virtual Slide
Note: Due to the technical difficulties of producing these slide preparations, the quality of these virtual slides is less than ideal.
1. Gingiva
There are three different stains: H&E, PAS & H, and Trichrome. These slides need some understanding of sectioning a three dimensional object in two dimensions! There is reasonable, undistorted tissue in some regions of these sections. Be sure you look at all three. The gingiva is the highly keratinized epithelium and underlying connective tissue lamina propria that surrounds the teeth. The extensive interdigitation with the lamina propria increases the surface area for epithelial attachment to the connective tissue. On one side of the section you can trace the transition from keratinized gingiva to nonkeratinized mucosa (in the PAS slide, some glycogen is stained in the mucosa).
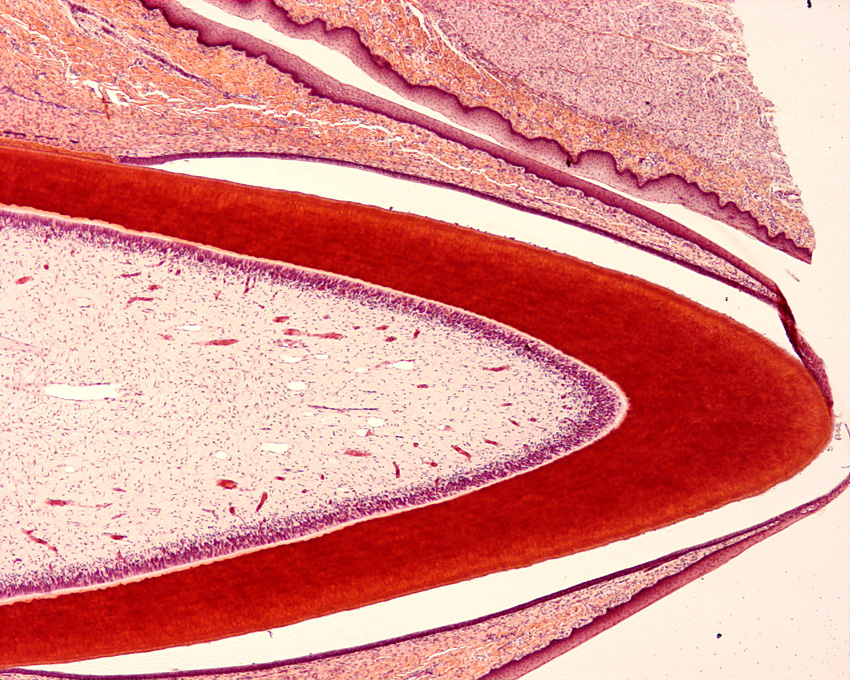
2. Tooth
The tooth in these sections lacks its outer layer of enamel because the tissue has been decalcified (recall that enamel is ~95% mineral); however, the matrix of the dentin is well preserved as is the cementum and adjacent matrix of the alveolar bone of the mandible. This is a multi-rooted tooth and very few slides exhibit the complete extent of the root. However, you should be able to see excellent regions of the periodontal ligament View Image connecting the root cementum to the alveolar bone. If you use a light microscope and close down the iris diaphragm you can see Sharpey’s fibers inserting into both the alveolar bone and root cementum. Note the extensive vascular supply to the periodontal ligament that travels in (an interconnected network of) loose connective tissue.
Find the cemento-enamel junction View Image and trace the acellular cementum toward the root apex where there is a transition View Image to cellular cementum [orientation]. The cellular cementum may be identified by the presence of cementocytes which, much like osteocytes, reside within lacunae (you will need to use your microscopes and glass slides to see this well). This monkey tooth has tortuous roots and the cellular cementum is usually present in a tangential section. In most sections, a series of longitudinally oriented increments of bone line the alveolar socket (where periodontal ligament fibers insert). Alveolar bone appears more like immature, or woven, bone and can be distinguished from the Haversian systems deeper within the bone, is particularly labile and is easily resorbed and deposited as a consequence of tooth movement. The dentinal tubules View Image can be seen in the dentin and, in many sections, distorted odontoblasts line the pulp cavity, which is otherwise filled with loose (almost mesenchymal) connective tissue. Odontoblasts and dentinal tubules can be seen very well in slide 123, which is of a tooth that is just about to erupt --ameloblasts can also be seen although the enamel is lacking since this section was also decalcified during processing.
The region of greatest clinical importance is the site of gingival attachment to the tooth View Image - again, since the enamel has been removed, the actual attachment cannot be seen, but you should be able to discern the approximate area where this occurs. This epithelial attachment to the enamel surface can break down leading to a chronic infection (periodontal disease). If the disease persists, the attachment epithelium and subjacent connective tissue become heavily infiltrated with white cells (you won’t see this in your slides as the tissue was healthy when the slides were prepared – you may see a few WBCs, but this is normal). The disease can progress resulting in loss of alveolar bone, periodontal ligament and, eventually, the tooth. Infections in this region can be important in patients with AIDS, patients receiving chemotherapy or radiation for cancer, and patients that have had a history of streptococcal and/or staphylococcal infections involving the heart, among others.
184 Tongue - Filiform papilla View Virtual EM Slide
Note the abundant deposit of keratin on the surface of the tongue and the characteristic shape of the filiform papilla show in this electron micrograph. Taste buds are NOT associated with filiform papillae.
185 Taste Bud View Virtual EM Slide
Note the difference in cell shape and cell aggregation of the taste bud and the oral epithelium. The nerve endings are sensory nerves. Be able to recognize a taste bud as such, but you will not be required to know its detailed structure and recognize different cell types.
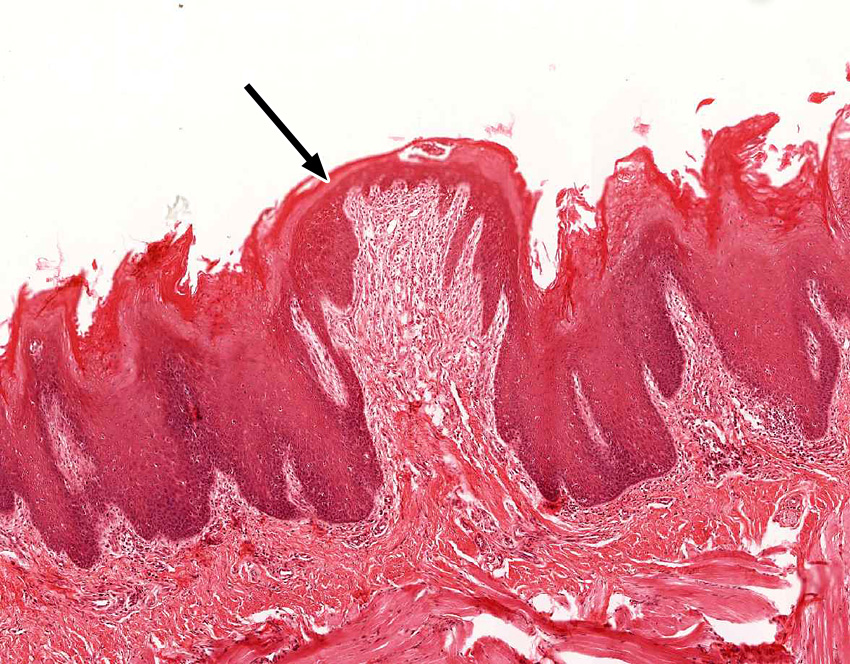
1. Where can the epithelium that is indicated by the black arrow be found?
- The vermillion zone of the lip
- A filliform papilla of tongue
- A fungiform papilla of tongue
- A circumvallate papilla of tongue
- The mucosa of pharynx
Answer
Correct answer 3. The structure shown is a fungiform papilla of tongue.
2. What does the periodontal ligament connect?
- Dentin to enamel.
- Dentin to cementum.
- Cementum to alveolar bone.
- Enamel to alveolar bone.
- The root of one tooth to the root of an adjacent tooth.
Answer
Correct answer 3. The periodontal ligaments are inserted in the cementum of teeth and in the alveolar bone.
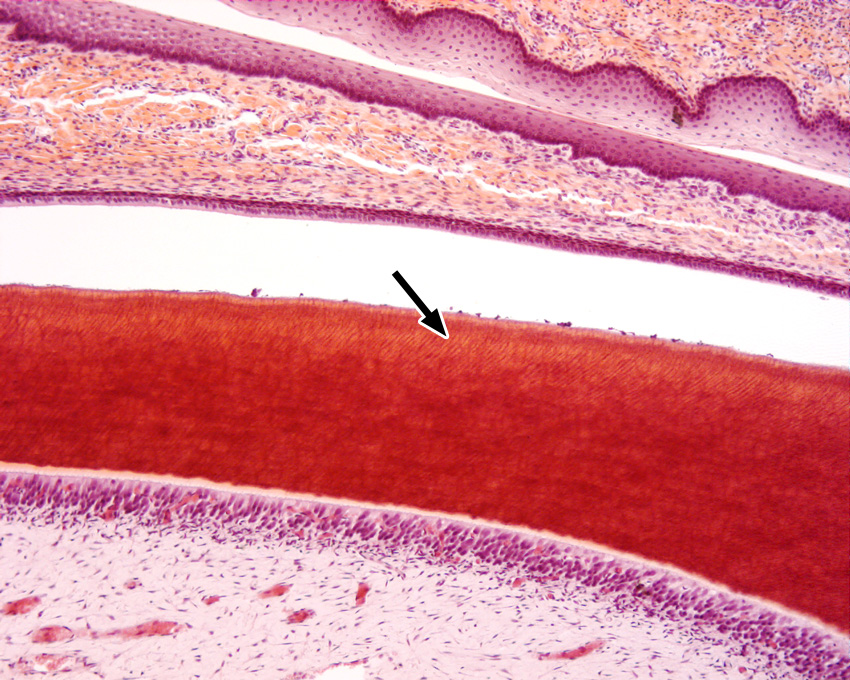
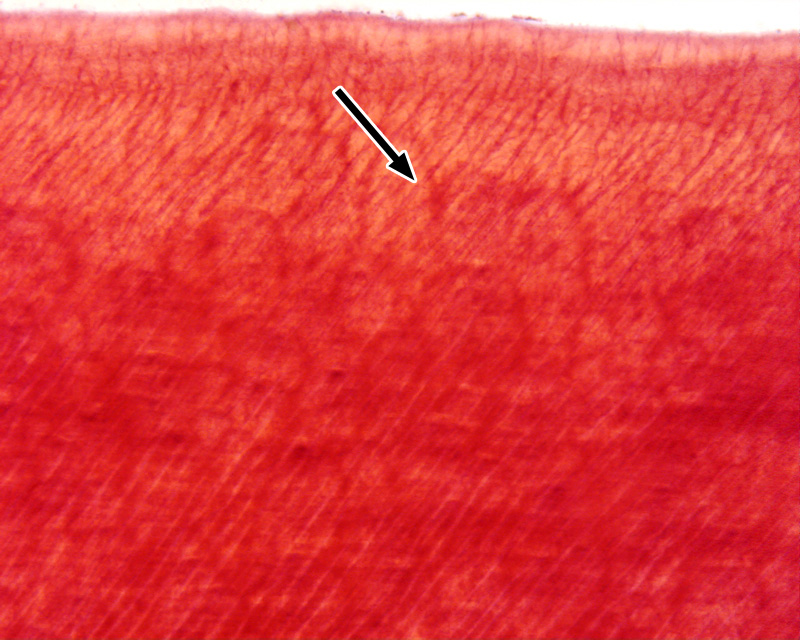
3. What does the tissue that is indicated by the black arrow contain?
- Cell processes of ameleoblasts
- Cell processes of odontoblasts
- Cell process of cementocytes
- Sharpey's fibers
- Capillaries from the pulp cavity
Answer
Correct answers 2. Dentin contains cell processes of odontoblasts. Remember that the enamel layer is not present in histological preparations.
Salivary Glands
1. Identify parotid, submandibular, and sublingual salivary glands on the basis of their histological appearance and by the type of secretion each gland produces.
2. Identify the three types of ducts (intralobular, intercalated, striated, interlobular) in salivary glands at the light microscope and the EM level and correlate their structural features with functional aspects of these ducts.
3. Know the localization of myoepithelial cells and nerves in relation to the acinar cells, and their role in secretory functions.
We will study three major salivary glands; the parotid, submandibular, and sublingual glands. These glands are divided into numerouslobules which contain the secretory units, which are called acini. Each secretory unit consists of acinar (secretory) cells and branching ducts. Ducts within lobules (intralobular ducts) connect with larger interlobular ducts which are found in the connective tissue between lobules.
Slide 184 Submandibular gland H&E View Virtual Slide
Tasks:
- find serous and mucous acini
- find serous demilunes
- find myoepithelial cells
Unlike the parotid gland, the submandibular and sublingual glands possess both mucous and serous secretory cells. Mucous cells have a pale-staining, bubbly cytoplasm and nuclei that appear to be pushed against the basal cell membrane. In contrast, the cytoplasm of serous cells contain distinctly eosinophilic zymogen granules and their nuclei are spherical in appearance. Compare the appearance of mucous and serous secretory cells and be sure you can tell the difference. The secretory cells are organized into secretory units or acini, and they are classified according to the cell types they contain:
- serous acini - contain only serous cells and are generally spherical
- mucous acini - contain only mucous cells and are generally tubular
- mixed (or sero-mucous) acini -contain a mixture of serous and mucous cells. In routinely-prepared tissue sections, the mucous cells swell and "push" the serous cells into a peripheral cap known as a serous demilune (demilune = "half-moon")
Slide 180-1 Parotid gland H&E View Virtual Slide
Slide 180-2 Parotid gland H&E View Virtual Slide
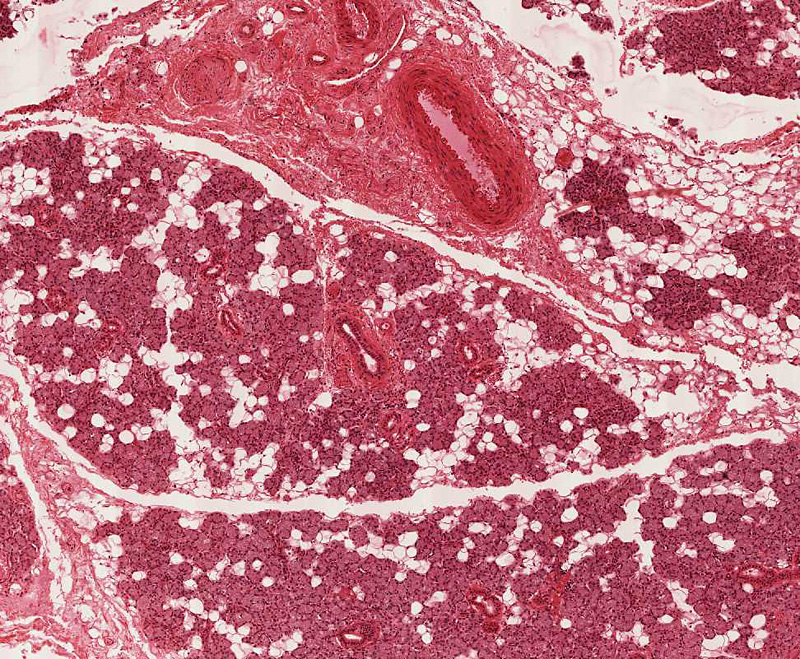
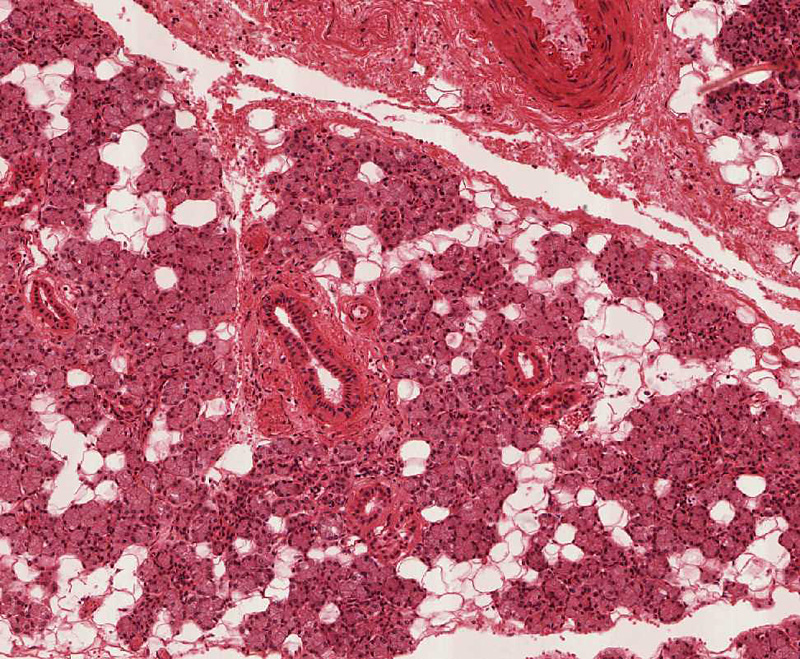
Using the low power objective, observe the abundance of fat in this gland: the amount of fat increases with age. Note that the parenchymal(secretory) tissue is divided into many lobules by the stromal (supportive) connective tissue. In this connective tissue stroma, notice the presence of blood vessels, nerves and large excretory ducts (interlobular). These interlobular ducts slide 180-2 View Image are lined by a pseudostratified columnar epithelium. Find a well defined lobule slide 180-2 View Image and observe the secretory acinar cells and ducts. You will note that these acinar cells are fairly uniform in size, structure and staining, because they all produce proteinaceous (serous) secretion. The secretory granules are not well preserved by routine methods of light microscopic fixation and are not recognizable in this slide.
With each lobule are intralobular ducts which are lined by a simple columnar epithelium of varying heights (becoming progressively taller toward the point at which the intraclobular ducts empty into interlobular ducts). The intralobular ducts are, in turn, further subdivided into striated and intercalated portions. Since the striated portions are much longer, you will see many more of them and we'll consider them first. Select a transverse section of a striated duct slide 180-2 View Image and observe the fine striations at the basal portions of the lining cells.
What are the "striations" of striated ducts?
Answer
The striations, noted with the light microscope, are due to vertical alignment of numerous long mitochondria in narrow compartments formed by deep invaginations (infoldings) of the plasma membrane at the cell base. These cytological specializations are for efficient active transport of water and ions to modify the primary secretion of the acini during its passage through this portion of the duct to a hypotonic solution containing high concentrations of bicarbonate.
The slender, intercalated ducts slide 180-2 View Image connect the secretory acini and striated ducts, but the intercalated ducts in this gland are much shorter than those in the pancreas (which we will cover in another session), so they are not as easy to spot.
Submandibular Gland:
Slide 183-1 Submandibular gland H&E View Virtual Slide
Slide 183-2 Submandibular gland (homo) 20X, mucicarmine stain [stains mucus red] View Virtual Slide
Slide 184 Submandibular gland H&E View Virtual Slide
Sublingual Gland:
Slide 185-1 Sublingual Gland 40X H&E View Virtual Slide
Slide 185-2 Sublingual Gland 40X H&E View Virtual Slide
Slide 185A Sublingual gland 20X mucicarmine and H&E stain [stains mucus red] View Virtual Slide
Unlike the parotid gland, the submandibular and sublingual glands possess both mucous and serous secretory cells. Slides 183-2 (submandibular) and 185A (sublingual) are stained with mucicarmine, which specifically stains mucus red. Survey the two alternate slides to compare the relative proportions of mucous acini in these two glands. After this, go back to the H&E-stained slides to study the histology of mucous and serous secretory acini.
In slide 183 and 184 of the submandibular gland, mucous secretory acini are those that stain lightly. Compare the appearance of mucous and serous secretory cells. The serous cells possess granular cytoplasm and nuclei which are spherical and vesicular in appearance. The mucous cells have pale staining cytoplasm and nuclei which appear to be pushed against the basal cell membrane. Now, observe the blind end of a mucous acinus and note the serous demilune cells View Image that cap this region of the secretory acinus. These demilune cells also have brightly staining granules in their cytoplasm. As an aside, the serous and mucous cells are actually adjacent to each other in vivo, and the formation of these demilunes is actually a fixation artifact (mucous cells swell with traditional fixation techniques and “squeeze out” the serous cells). Even so, the characteristic appearance of demilunes is nonetheless a useful diagnostic for identifying sero-mucous glands. Switch to a lower power and observe the distribution of ducts. Note the presence of large ducts in the connective tissue septae separating the lobules. These are interlobular or excretory ducts View Image and their epithelium appears to be stratified. The intralobular ducts within the lobules are smaller and similar in appearance to those of the parotid gland (i.e. they are striated ducts). The intercalated ducts in the submandibular and sublingual glands are very short and therefore NOT encountered often in sections.
Now examine slide 185-1 and 185-2, the sublingual gland, and note the greater prominence of mucous acini and fewer numbers of intralobular ducts than in the submandibular gland. Some lobules in slide 185-1 and 185-2 reveal almost all ducts with a few remaining secretory cells. This represents a pathological transformation of secretory acini to duct-like structures.
187 Glands - Lingual Mucous Glands Mucous Acinus of a Lingual Salivary Gland View Virtual EM Slide
Note the accumulation of mucin-containing secretory vesicles next to the lumen of the secretory acinus depicted in this electron micrograph.
Click on a question to reveal the answer.
What are the "striations" of striated ducts?
The striations, noted with the light microscope, are due to vertical alignment of numerous long mitochondria in narrow compartments formed by deep invaginations (infoldings) of the plasma membrane at the cell base. These cytological specializations are for efficient active transport of water and ions to modify the primary secretion of the acini during its passage through this portion of the duct to a hypotonic solution containing high concentrations of bicarbonate.