- Understand the general organization of the kidney, be able to differentiate cortex from medulla, and know the blood supply of the kidney.
- Know the structural organization of a generic nephron, its parts, where each part/section is located (cortex vs. medulla) and be able to recognize them at the light and EM level (renal corpuscle, proximal and distal convoluted tubules, loop of Henle, and collecting tubules/ducts, which are shared by multiple nephrons).
- Know and identify the structures/cells of renal corpuscles and how they constitute the renal filtration barrier to produce a blood plasma filtrate.
- Describe how the tubular segments of nephrons and collecting tubules/ducts modify the filtrate to produce urine.
- Know and recognize important structures that are involved in the control of renal function, the regulation of blood pressure, and how they are controlled by hormones (ADH and aldosterone).
- Be able to recognize transitional epithelium (relaxed only), know how it functions, and the histological structure of the bladder.
In this laboratory you will study the kidney, ureter and bladder. Your main goal in the kidney will be to understand how blood vessels and nephrons are organized in the kidney cortex and medulla, and how this arrangement is related to the production of urine. The nephron consists of a renal corpuscle (the glomerulus and Bowman's capsule), a proximal tubule (with convoluted and straight portions), a thin segment, and a distal tubule (with straight and convoluted portions). The nephron empties into a collecting duct. You will not be able to see a nephron in its entirety in a single section, but will study the various portions separately in the slides below. Unfortunately, the kidney is difficult to fix optimally, and so you will look at several kidney slides, each of which may show one aspect or another to better advantage. The quality of fixation may even vary somewhat in different parts of the same section, so look around for a moment before you settle down to study structures.
Slide 204 kidney H&E View Virtual Slide
Slide 210 kidney monkey H&E View Virtual Slide
Slide 210 kidney monkey PAS/Pb hematoxylin View Virtual Slide
Part of a human kidney in cross-section is shown in slide 204. One side of the section is relatively smooth and convex; this is the outer surface of the kidney. Underlying that surface (capsule) is a layer of cortex slide 204 View Image about 5 mm thick. Most of the remainder of the section is the medulla in slide 204 View Image, forming renal pyramids (roughly triangular in appearance). The apex (tip) of the pyramid forms the papilla slide 204 View Image.
The short red strips, which you may see in the medulla in slide 204 View Image are "vasa recta" (see section "C" below for more discussion of the kidney vasculature). The monkey kidney (slide 210) is a "unipyramidal" type-it has only one pyramid; the human has many. The monkey kidney was perfused and most of the RBCs have been washed out, but the histology is excellent and the diameter of tubules is close to that in real life.
A. Cortex
Examine the cortex of slide 204. You will recognize medullary rays (or pars radiata) in slide 204 View Image, which are clusters of parallel tubules (sectioned longitudinally) that appear to be coming out from the medulla. The region of cortex between the rays, called the cortical labyrinth (or pars convoluta) in slide 204 View Image, contains renal corpuscles and the convoluted portions of the tubules.
1. Tubules
Identify the three general types of tubules that occur in the cortical labyrinth and medullary rays of the cortex:
- proximal tubules (further sub-divided into convoluted and straight portions),
- distal tubules (also divided into convoluted and straight portions), and
- collecting tubules (or ducts).
The preservation of tissue varies between the two slides. A certain degree of distortion and tissue breakdown exists and it will be necessary to study both slides for the best histology of the tubules. Most of the tubules you see in the cortical labyrinth in slide 204 View Image and slide 210 View Image are proximal convoluted tubules, which are large, prominent and generally stain a deeper pink than the other tubules. As an artifact of histological preparation, in some sets there may be small, white splits in the walls of these tubules, which should be ignored. In the cortex in slide 204 View Image, the straight portion of the proximal tubule is in the medullary rays, and has a similar histological appearance to proximal convoluted tubules. It is difficult to have the brush border (composed of microvilli) well preserved in microscopic preparations. The brush border on the luminal surface of the proximal tubule epithelium in slide 204 is less well preserved than in slide 210 and tends to slough off and partly fill the lumen as pink material. In slide 210-PAS, stained with periodic acid-Schiff reagent, there is good preservation and staining of the brush border. Be sure you actually see the brush border. In addition, the basement membranes associated with the epithelial linings of blood vessels, Bowman capsules, and tubules are distinct in slide 204 View Image.
Here and there among the proximal tubules in the cortical labyrinth you will also see distal convoluted tubules in slide 204 View Image and slide 210 View Image. You should note that distal tubules are paler in appearance, usually have a smaller diameter, and a low cuboidal epithelium. In the cortex, the straight portion of the distal tubule slide 204 View Image is similar in appearance and occurs in the medullary rays.
The third type of tubule in the cortex is the collecting duct (or tubule), which is also best seen in the medullary rays in slide 204 View Image and slide 210 View Image. Look for tubules in which the epithelium is simple cuboidal or low columnar, the cell outlines usually appear particularly distinct, and the nuclei are prominent and closer together than in proximal or distal tubules. Be sure you can identify each of the three types of straight tubule found in a medullary ray slide 210 View Image (proximal straight, distal straight, and collecting tubules). Collecting tubules may also be seen occasionally in the cortical labyrinth. Numerous capillaries occur between the tubules in the cortex. In slide 204, note the outlines of red blood cells in slide 204 View Image in these small vessels. The kidney in slide 210 was perfusion-fixed and, therefore, the capillaries are devoid of red blood cells.
2. Renal Corpuscle
Examine the renal corpuscles found in the cortex, noting the numerous capillary loops of the glomerulus slide 210 View Image. Most of the flat nuclei in the glomerulus belong to endothelial cells and to podocytes (simple squamous epithelium constituting the visceral layer of Bowman's capsule). Some nuclei in the central regions of the glomerulus may belong to mesangial cells.
What are the three layers involved in glomerular filtration and how do they work?
Answer
There are three layers that make up the filtering system of the glomerulus. These are the capillary endothelium, the glomerular basement membrane (made of the fused basement membranes of the endothelial cells and podocytes) and the podocyte layer. Renal capillaries are fenestrated capillaries without diaphragms. They are covered with podocalyxin, a negatively charged molecule. Their negative charge helps prevent negatively charged molecules pass through the filter. Between the podocytes and fenestrated capillary endothelial cells of the kidney there is a fused basal lamina made of two lamina rara and a single lamina densa (the glomerular basement membrane). Embedded in the lamina densa are molecules of perlecan, which is made up of negatively charged heparin sulfate chains. The lamina rarae are particularly rich in such polyanions, so they contribute significantly to this charge exclusion filter which prevents negatively charged molecules from passing through. The collagen IV and laminin meshwork of the lamina densa serves as a size barrier, helping to prevent the passage of proteins through the filter. The secondary processes of the podocyte interdigitate to form filtration slits with diaphragms between them. They are also covered with podocalyxin that helps keep the processes apart and also serves as a last effort to prevent the filtration of negatively charged molecules. They also prevent large molecules (like proteins) from coming through. Their main purpose, however, is to regulate water flow.
Note that we do not expect you to be able to distinguish among these 3 cell types by light microscopy. The parietal layer of Bowman's capsule is also a simple squamous epithelium which transitions to cuboidal epithelium of the proximal convoluted tubule at the urinary pole slide 210 View Image. Look around under low power to find glomeruli sectioned through the vascular pole. Near the vascular pole will be the distal tubular part of the same nephron. Some sections in slide 204 View Image and slide 210 View Image will show a portion of this distal tubule with unusually closely packed nuclei. This region is the macula densa which is located at the end of the ascending straight tubule where the distal convoluted tubule begins slide 210 View Image. The macula densa together with the juxtaglomerular cells and the extraglomerular mesangial cells (lacis cells) form the "juxtaglomerular apparatus". Juxtaglomerular cells are specialized smooth muscle cells found in the wall of the afferent (and to some extend the efferent) arteriole which secrete renin. You cannot distinguish juxtaglomerular cells in these preparations (but you could detect them by immunological techniques, e.g., immunostaining for renin).
B. Medulla
Move to the medulla slide 210 View Image, where straight proximal and distal tubules as well as collecting ducts are found. Blood vessels (note outlines of red blood cells in slide 204) are also seen. In the medulla is the loop of Henle, usually composed of:
- An initial thick portion that represents the continuation of the straight proximal tubule from the medullary ray,
- A thin descending portion that turns back toward the cortex as a thin ascending portion that is continuous with
- A thick ascending portion, which is a segment of the straight distal tubule.
The thick portions have an histology characteristic of either proximal or distal tubule. The thin portion is lined by a simple squamous epithelium and cannot reliably be distinguished from capillaries (unless blood cells are present in the capillaries as in slide 204 View Image). The deepest portions of the medulla have only thin segments and collecting ducts. The epithelium of the collecting ducts becomes higher as these ducts pass toward the papilla (where they are called "papillary ducts" or ducts of Bellini slide 210 View Image). As an artifact in some slides, the collecting duct epithelium may be pulled away from its basement membrane in some areas of the papilla, leaving a white space between the epithelium and its underlying connective tissue. Urine is released at the papilla through 10-25 openings (area cribrosa) into one of the minor calices which you will note are lined with transitional epithelium slide 210 View Image (somewhat damaged in slide 204 View Image) as is the rest of the urinary tract. It is worth noting that, from this point onward, the osmolarity of the urine can no longer be modified since transitional epithelium is essentially impermeable to salts and water.
C. Blood Supply
Now that you have seen the arrangement of various nephron components in the kidney, go back and follow the blood supply. Slide 204 is helpful to study the blood supply even though the tubular epithelium in this slide is in bad shape! You will remember from gross anatomy that the renal artery enters the hilus of the kidney, and divides successively into lobar, interlobar (these are difficult to identify with certainty in histological sections, but they are the large arteries among the pyramids that are upstream of the arcuate arteries) and finally into arcuate arteries, which are accompanied by the corresponding veins.
Observe interlobar arteries and veins in slide 204 View Image, sizable vessels passing along the lateral sides of the medullary pyramid. Arcuate arteries and veins follow the base of the medullary pyramid along the boundary between the renal medulla and the renal cortex. From the arcuate arteries, relatively straight branches, the interlobular arteries and vein slide 204 View Image extend up between the lobules of the cortex where they branch off into the intralobular arteries and, in turn, the afferent arterioles in slide 210 View Image that supply the glomeruli within each lobule. Human kidneys do not have interlobular arteries, just afferent arterioles. Even though most of the RBCs have been washed out of the tissue in slide 210, the arcuate and interlobular vessels should still be identifiable by the smooth muscle in their walls (also, note that arcuate vessels are generally lining the base of the medullary pyramid along the cortico-medullary boundary).
Efferent arterioles (do not worry about distinguishing between afferent vs. efferent arterioles), leaving the glomeruli, divide into peritubular capillaries which may be seen as small circular profiles amongst all the convoluted tubules. The majority of these capillaries then coalesce to enter the interlobular veins, allowing the blood to pass back to the general circulation. However, efferent arterioles from some glomeruli near the medulla (i.e., juxtamedullary glomeruli) provide the blood supply for the medulla. The multiple small vessels (arterioles that are more like dilated capillaries) arising from the efferent arterioles and descending into the medulla and the somewhat larger venules ascending from it are clustered to form the vasa recta, which you observed earlier in slide 204 as radiating reddish (or brownish) stripes in the medulla. The close association of arterioles and venules in the vasa recta provide counter-current exchange to help prevent loss of the high electrolyte concentration present in the inner medulla, necessary for the concentration of urine. Capillaries receiving blood from arterioles of the vasa recta are seen throughout the lower medulla. The venules of the vasa recta empty into arcuate or interlobular veins.
Explain the flow of blood through the kidney
Answer
Blood enters the kidney through the large renal arteries. At the hilum, the renal arteries branch and become interlobar arteries. Interlobar arteries travel through the medulla to the corticomedullary junction where the arteries branch into arcuate arteries that run along the corticomedullary junction. The arcuate arteries further branch and become interlobular arteries that run through the renal cortex. From the interlobular arteries come afferent arterioles that become the glomerulus. Exiting from the glomerulus is the efferent arteriole. After leaving glomeruli in the cortical region, the efferent arteriole leads to the peritubular capillary network. Efferent arterioles of the juxtamedullary glomeruli become the vasa rectae, which can be seen in the medulla. The vasa rectae and peritubular capillary network drain directly into interlobular veins. Peritubular capillaries drain into stellate veins and then into interlobular veins. From there blood travels to the arcuate veins, interlobar veins and finally leaves through the renal vein.
Other Potentially Useful Kidney Slides
Slide 203N kidney H&E tangential View Virtual Slide
This section of kidney cortex was cut parallel to the surface of the kidney, and thus shows medullary rays in cross section in View Image. Observe such rays to see cross sections of straight proximal and distal tubules as well as collecting ducts. Also, you may have a more favorable view of maculae densae in this slide.
Slide 209 kidney monkey including pelvis H&E View Virtual Slide
In this cross section of a monkey kidney, you will recognize cortex at the periphery and a medullary pyramid in the center. Review some of the features of kidney structure you saw in slides 204 & 210. Many of the tubules in the cortex are swollen, making it somewhat more difficult to distinguish proximal tubules from distal and collecting tubules. However, you may find structures in the medulla somewhat easier to interpret than those of slides 204 & 210.
Slide 205 kidney monkey vascular injection H&E View Virtual Slide
An opaque red gelatin was injected through the renal artery of this kidney, filling many of the arteries and capillaries. Observe the distribution of blood vessels. It may require some insight to orient yourself on this section, since some of the cortex has been removed during preparation of the section. The vasa recta in slide 205 View Image are interesting here, since the descending arterioles are injected but the ascending venules did not receive the injection material and are full of red blood cells, which appear yellow.
Slide 206 kidney 200mm crown-rump length H&E fetal View Virtual Slide
Here you see a stage in kidney development. The kidney lobes (pyramids and their associated cortex) are particularly obvious at this stage of development, but eventually fuse to yield a smooth capsule with portions of each lobe forming the renal columns. You do not need to study this section in detail. The various components you have seen in previous slides are here, but in rudimentary form. One particular advantage to this section is that the RBCs are not washed out of the tissue and developing tubules in the medulla are separated quite nicely by connective tissue, so it is quite easy to discern vasa rectae, collecting tubules, and thick and thin portions of Henle's loops in slide 206 View Image. In this section you can also see an arcuate artery (which arches along the cortico-medullary boundary) arising from an interlobar artery in slide 206 View Image.
Slide 211 ureter ureter H&E View Virtual Slide
Slide 019-1 ureter rat over-distended H&E View Virtual Slide
Slide 019-2 ureter rat non-distended H&E View Virtual Slide
In these cross-sections of the ureter, note the transitional epithelium lining the lumen in slide 211 View Image. You studied the transitional epithelium (in slide 19), in relaxed and stretched states, in a previous laboratory period dealing with epithelia. There are 2 to 3 layers of smooth muscle in the ureter. However, the smooth muscle is arranged in bundles that make the layers appear somewhat disorganized, thus it may be difficult for you to distinguish them. The connective tissue between the epithelium and the muscle is considered to be a lamina propria (there is no submucosa). There is an adventitia (connective tissue) outside the smooth muscle.
B. Bladder
Slide 212 bladder View Virtual Slide
Duke University slide 98, (non-distended bladder, H&E) View Virtual Slide (virtual slide courtesy of Duke University)
Compare the size of the bladder to that of the ureter and note that it is also lined with transitional epithelium in slide 211 View Image. You will remember that transitional epithelium is remarkable for its ability to stretch and yet maintain a strong barrier to diffusion of components in the urine. The muscular wall of the bladder, made up of bands of smooth muscle, provides for the expulsion of the urine during urination. Although three muscular layers are sometimes described in textbooks, they are usually rather difficult to distinguish in histological sections.
165 Kidney - Glomerulus View Virtual EM Slide
Study the architecture of the glomerulus in this section of renal corpuscle. Review the organization and function of the glomerular endothelium, basement membrane and the podocytes. (The vascular pole is included in the plane of section, but not the urinary pole. The juxtaglomerular cells are secretory cells, derived from smooth muscle cells of the afferent arteriole. The macula densa shown here is cut in tangential section passing only through its wall and does not include the lumen (the rest of the tubule is out of the plane of section). You can at least see the closely-packed nuclei that are characteristic of this modified portion of the distal tubule.
166 Kidney - Glomerulus Detail View Virtual EM Slide
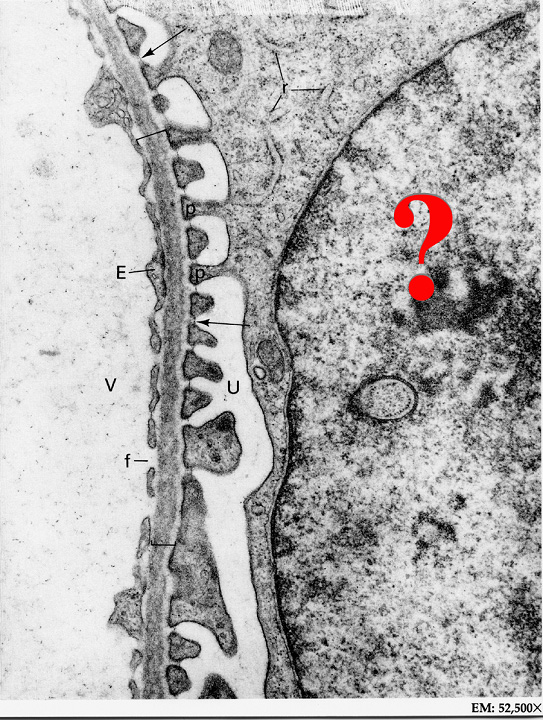
Review the components of the glomerular filtration barrier and note that poodocytes and their foot processes (pedicels) form the visceral layer of the Bowman’s capsule.
170 Kidney - Cortex, proximal tuble Brush Border View Virtual EM Slide
This EM micrograph depicts the typical appearance of microvilli on the apical surface of two types of cells with a striated or brush border. Shown is the epithelial lining cell of a proximal tubule in the kidney.
172 Kidney - Distal Convoluted Tubule View Virtual EM Slide
Compare the distal convoluted tubule shown here with the proximal tubule seen in the previous micrograph. Note that, like the epithelial cells of the proximal convoluted tubule, these there are also abundant mitochondria (which you would expect since these cells are involved in the active transport of sodium). However, there are very few microvilli.
175 Kidney - Loop of Henle View Virtual EM Slide
Note the abrupt transition of the epithelium lining thin segment to thick segment of the loop of Henle.
182 Kidney - Papillary Collecting Duct Papillary Collecting Duct (Duct of Bellini, cross section) View Virtual EM Slide
The cells of the collecting duct grow taller as the duct approaches the renal papilla.
183 Urinary Bladder – Section of Wall Transitional Epithelium View Virtual EM Slide
Transitional Epithelium. This micrograph displays the transitional epithelial lining of the bladder. The wall of the urinary bladder contains 3 layers of somewhat irregularly arranged smooth muscle.
Click on a question to reveal the answer.
What are the three layers in glomerular filtration and how do they work?
There are three layers that make up the filtering system of the glomerulus. These are the capillary endothelium, the glomerular basement membrane (made of the fused basement membranes of the endothelial cells and podocytes) and the podocyte layer.
Explain the flow of blood through the kidney
Blood enters the kidney through the large renal arteries. At the hilum, the renal arteries branch and become interlobar arteries. Interlobar arteries travel through the medulla to the corticomedullary junction where the arteries branch into arcuate arteries that run along the corticomedullary junction. The arcuate arteries further branch and become interlobular arteries that run through the renal cortex. From the interlobular arteries come afferent arterioles that become the glomerulus. Exiting from the glomerulus is the efferent arteriole. After leaving glomeruli in the cortical region, the efferent arteriole leads to the peritubular capillary network. Efferent arterioles of the juxtamedullary glomeruli become the vasa rectae, which can be seen in the medulla. The vasa rectae and peritubular capillary network drain directly into interlobular veins. Peritubular capillaries drain into stellate veins and then into interlobular veins. From there blood travels to the arcuate veins, interlobar veins and finally leaves through the renal vein.
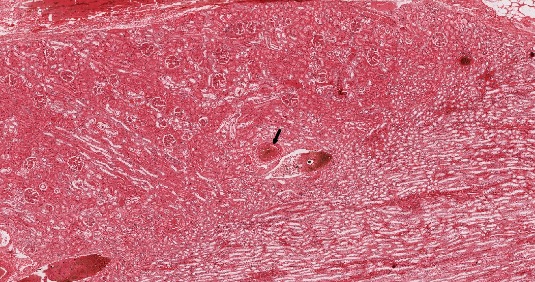
1. Identify the structure indicated by the black arrow.
- An interlobar artery
- An interlobar vein
- An arcuate artery
- An arcuate vein
- An interlobular artery
- An interlobular vein
Answer
Correct answer 3. An arcuate artery- the vessel is definitely an artery of some sort (note the smooth muscle layers and internal elastic lamina) and it is located at the cortico-medullary junction, which is where arcuate arteries are found.
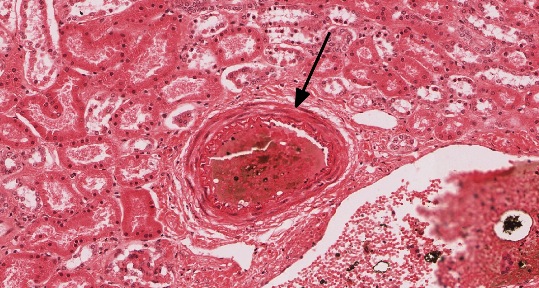
2. Identify the structure indicated by the black arrow.
- A proximal convoluted tubule
- A distal convoluted tubule
- A proximal straight tubule
- A distal straight tubule
- A cortical collecting duct
- A medullary collecting duct
Answer
Correct answer 6. A medullary collecting duct- note that the lateral border of each cell is clearly demarcated, a key feature of collecting ducts. Specifically, the duct is in the MEDULLA, which is evident because there are NO convoluted tubules or glomeruli present. Note also that there are also thin loops of Henle around, which are mostly only in the medulla. Lastly, as the collecting duct extends from medullary rays in the cortical region down into the medulla, the cells become more columnar as seen here.
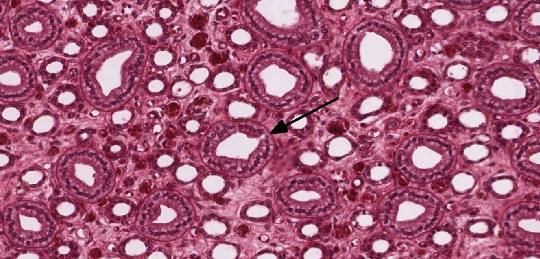
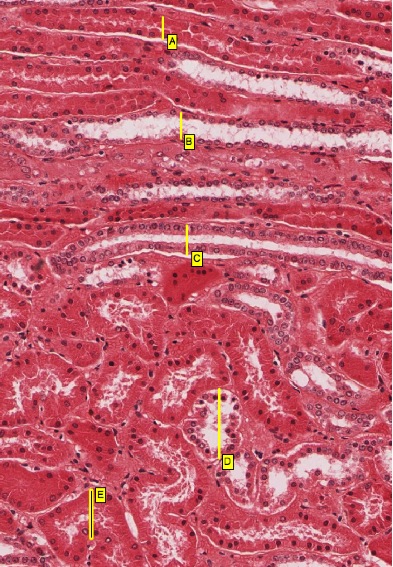
3. Which of the indicated tubules is generally the MOST permeable to water?
- A
- B
- C
- D
- E
Answer
Correct answer 5. (E). Proximal convoluted tubules are lined by epithelial cells that constitutively express aquaporin channels and are therefore generally the MOST permeable to water. "A" is a proximal straight tubule. "B" is a distal straight tubule. "C" is a cortical collecting duct, which, under the influence of ADH, can become water permeable, but not to the same extent as a proximal convoluted tubule (A, B, and C are all in a medullary ray). "D" is a distal convoluted tubule.
4. Name the cell that is indicated by the question mark.
- A juxtaglomerular cell
- A macula densa cell
- A mesangial cell
- A podocyte
- A parietal epithelial cell of Bowman's capsule
Answer
Correct answer 4. A podocyte - Note that you can see areas where the cytoplasm of the cell is connected to the pedicels (foot processes, labeled "p"). "V" labels vascular lumen. "E" indicates endothelial cell cytoplasm. "f" indicates an endothelial fenestra. The bracket indicates basal lamina. "U" indicates urinary space. The arrow indicates a filtration slit (covered by a diaphragm). "r" indicates ribosomes on rough ER.
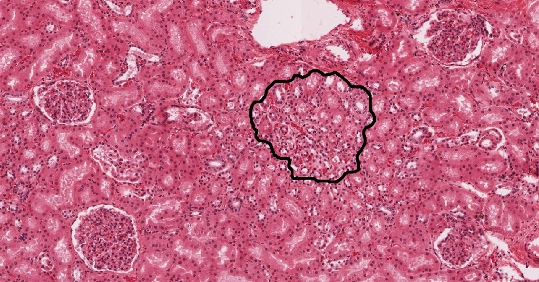
5. Compared to blood plasma osmolarity (~300 mOsm), what is the osmolarity of the interstitial fluid within the indicated area?
- Hypo-osmotic
- Iso-osmotic
- Hyper-osmotic (600 milliosmoles)
- VERY hyper-osmotic (1200 milliosmoles)
Answer
Correct answer 2. Iso-osmotic - the outline indicates a medullary ray (note the collecting duct at about 2 o'clock). However, note that it is in the CORTEX of the kidney (observe the surrounding glomeruli and convoluted tubules) and, like the rest of the cortex, the fluid in the interstitium here is iso-osmotic.
6. Which statement(s) is/are correct about transitional epithelium?
- It is found only in the ureters and bladder.
- It is freely permeable to water.
- It is freely permeable to salt ions.
- ALL of the above statements are correct.
- NONE of the above statements are correct.
Answer
Correct answer E. NONE OF THE ABOVE. Transitional epithelium is also found in the calyxes of the kidney and the superior urethra. It is completely impermeable to water and salt.
7. Which of the labeled ultrastructural features most significantly impedes the passage of negatively charged molecules?
- A
- B
- C
- D
Answer
Correct answer 4. (D). The lamina rara interna and externa contain an extensive amount of negatively charged proteoglycans which therefore REPELS negatively charged molecules and impede their passage into the urine filtrate.