- Know the basic components of the conducting and respiratory portion of the respiratory system and describe distinctive structural features of each component related to its particular function in respiration.
- Know the types of cells present in the respiratory epithelium and their functions.
- Be able to identify the trachea, bronchi, bronchioles/terminal bronchioles, respiratory bronchioles, alveolar ducts and alveoli on the basis of epithelial cell types present, and relative amounts of glands, cartilage, smooth muscles, and connective tissue fibers present in the wall of the tubes.
- Be able to identify the components and cells of the alveolar space and the alveolar wall and know their respective function (type 1 and 2 pneumocytes, surfactant, alveolar macrophages, alveolar capillaries).
- Be able to name and identify the structural elements that form the blood-air barrier.
- Know the vascular supply of a lung and be able to identify pulmonary arteries, pulmonary veins, and the bronchial arteries and whether they contain oxygenated or deoxygenated blood.
For descriptive purposes the respiratory system is divided into (a) conducting and (b) respiratory portions. The conducting part consists of passageways which carry air to the respiratory portion. The respiratory portion begins at the level where alveoli first appear in the final branches of the bronchioles. Respiration (gaseous exchange between blood and air) occurs across the walls of the alveoli. The conducting portion includes parts which are outside the lung or extrapulmonary (nasal cavities, nasal pharynx, larynx, trachea and primary bronchi), and those which are inside the lung or intrapulmonary (rest of the bronchi and bronchioles). All of the respiratory portion is, of course, intrapulmonary and consists of the respiratory bronchioles, alveolar ducts, and alveoli). Click here to see a diagram summarizing the histological organization of the respiratory system.
A. Nasal Cavity
Slide 124 (nasal cavity, frontal sect., monkey, H&E) View Virtual Slide
Slide 124F (nasal vestibule, frontal sect., monkey, H&E) View Virtual Slide
Slide 124P (post. nasal cavity, frontal sect., monkey, H&E) View Virtual Slide
Slide 124-O (post. nasal cavity, frontal sect., monkey, H&E) View Virtual Slide
Slide 115 (fetal palate, sag. sect, H&E) View Virtual Slide
We will look at a frontal section of the nose (slide 124). Identify the palate, nasal septum and nasal cavities. The epithelial lining at the entrance (vestibule) to the nasal cavity exhibits a gradual change from keratinized stratified squamous epithelium of the skin in the nasal vestibule (shown in slide 124F) View Image, to the pseudostratified columnar ciliated epithelium that is characteristic of the nasal mucosa posterior to the vestibule (shown in slides 124 and 124P) View Image and much of the rest of the respiratory system. Therefore, the epithelium is called respiratory epithelium. Note, slides 124F, 124, and 124P were cut in the FRONTAL (coronal) plane, so you will NOT be able to see the actual transition from squamous to respiratory epithelium in the nasal cavity (to see this transition, you would need a sagittal section). Slide 124F is the anteriormost of these sections (the teeth that can be seen below the nasal cavity are incisors) and lining of the nasal cavity is entirely stratified squamous epithelium. Slides 124 and 124P are more posterior sections (the teeth in these slides are molars), so the lining present in these slides is pretty much entirely respiratory epithelium. Olfactory epithelium, specialized for smell, lines the roof of the nasal cavity and can be seen very well in slide 124-O View Image and somewhat in slide 124 View Image. This region may be recognized by the dramatically thickened epithelium which LACKS goblet cells. Beneath the olfactory epithelium are numerous nerve fibers which are branches of the olfactotry nerve as well as specialized olfactory glands (Bowman’s glands), the secretions of which are “serous” (mostly water and some protein) rather than mucous. The watery secretions dissolve odorant molecules to facilitate their detection and then quickly wash the odorants away so that new scents can be detected. The nasal mucosa lining the bulk of the nasal cavity is made up of respiratory epithelium and an underlying layer of connective tissue View Image. The connective tissue contains many glands (and associated ducts) and a rich vascular plexus characterized by many dilated, thin walled veins (sometimes called "venous spaces") which act as heat exchangers to warm and humidify the air entering the nasal cavity. Now look at a sagittal section of the palate (slide 115) and compare respiratory epithelium of the nasal passage View Image to the stratified squamous epithelium of the oral cavity.
B. Larynx (W pg 237, 12.5)
Slide 125-1 (larynx, sag. sect., H&E) View Virtual Slide
Slide 125-2 (larynx, sag. sect., H&E) View Virtual Slide
Slide 125-3 (larynx, sag. sect., H&E) View Virtual Slide
The mucosal surface of the rest of the conducting portion is lined by respiratory epithelium, except the true vocal fold (vocal cord or vocal ligament) View Image in the larynx, which is lined by a stratified (sometimes keratinized) squamous epithelium. The upper false vocal fold(vestibular or ventricular fold) View Image is covered by respiratory epithelium, which makes an abrupt transition to a stratified squamous epithelium over the true vocal fold. The stratified epithelium serves to protect the vocal cords from abrasion caused by vibrations of the true vocal folds during phonation. Also, note that the cores of the upper (false) folds contain numerous muco-serous secretory glands (the serous components stain evenly whereas the mucous cells have a bubbly appearance) View Image , while the cores of the lower (true) focal folds contain elastic fibers and skeletal muscle (vocalis muscle) View Image cut in cross section (the elastic fibers will appear as dots in the extracellular matrix).
C. Trachea (W pgs 226-7)
Slide 40 (trachea, H&E) View Virtual Slide
Slide 126 (trachea & esophagus, cross sect, H&E) View Virtual Slide
Slide 127 (trachea, cross sect., trichrome) View Virtual Slide
The epithelium lining the trachea is typical respiratory epithelium (ciliated pseudostratified columnar) View Image, which, like the nasal epithelium, contains numerous goblet cells. This epithelium has an unusually thick basement membrane, which you can see as a narrow pink-staining region immediately basal to the epithelium. This epithelium plus its underlying layer of loose connective tissue (the lamina propria) make up the tracheal mucosa. The layer under the mucosa is the submucosa wherein you'll find numerous sero-mucous glands View Image. The mucosa is separated from the submucosa by a layer of longitudinal elastic fibers. This elastic layer is often not obvious in your sections, so we do not require you to decide where the division occurs. However, as you may recall from the connective tissue lab session, slide 40 happens to show these fibers quite well (cut in cross section, so they appear as eosinophilic, glass-like dots) View Image. Outside the connective tissue layers, observe the C-shaped rings of hyaline cartilage View Image which help to keep the lumen of the trachea from collapsing. It is unlikely that your histological section will follow the same C-shaped ring all the way around the trachea; instead, it will probably pass in and out of two or more rings. The ends of the rings are bridged by horizontally oriented smooth muscle (the trachealis muscle) View Image, which can act to adjust the diameter of the trachea. This muscle is seen especially well in those examples of slide 127 that are stained with Masson's trichrome View Image. Outermost is a layer of connective tissue, the adventitia.
Slide 129_20x (lung, H&E) View Virtual Slide
Slide 130_20x (lung, H&E) View Virtual Slide
Slide 130-1_40x (lung, H&E) View Virtual Slide
Slide 130-2_40x (lung, H&E) View Virtual Slide
Slide 132_20x (lung, H&E) View Virtual Slide
Slide 132_40x (lung, H&E) View Virtual Slide
A. Bronchi The trachea bifurcates into two primary bronchi, which enter the lung and then branch several times to give rise to smaller secondary and tertiary bronchi View Image. Bronchi differ from the trachea in having plates rather than rings of cartilage, and in having a layer of smooth muscle between the lamina propria and submucosa. In smaller branches, the amount of cartilage decreases, whereas the amount of smooth muscle increases. Also, the number of glands and goblet cells decreases. Don't worry about trying to distinguish among primary, secondary, and tertiary bronchi, but you should be able to distiguish bronchi in general from the trachea and bronchioles (discussed below).
B. Bronchioles Bronchioles View Image are smaller branches of the bronchi, and are distinguished from them by the absence of cartilage and glands. In larger bronchioles, the epithelium is still ciliated, but is now usually simple columnar, whereas in the smallest bronchioles, the epithelium will be simple cuboidal (mostly club cells, formerly known as Clara cells) and lack cilia altogether. The smooth muscle layer is generally quite prominent in these structures as demonstrated in slide 132-2 View Image where the bronchiole was cut in a grazing longitudinal section allowing you to see the circularly arranged bundles of smooth muscle in the bronchiolar wall. As mentioned above, the smallest conducting bronchioles consist of a simple cuboidal (or perhaps "low columnar") epithelium of mostly club cells, a few ciliated cells, and NO goblet cells, and are called terminal bronchioles View Image.
Slide 129_20x (lung, H&E) View Virtual Slide
Slide 130_20x (lung, H&E) View Virtual Slide
Slide 130-1_40x (lung, H&E) View Virtual Slide
Slide 130-2_40x (lung, H&E) View Virtual Slide
Slide 132_20x (lung, H&E) View Virtual Slide
Slide 132_40x (lung, H&E) View Virtual Slide
A. Respiratory Bronchioles You might see short, transitional regions of bronchioles which have a few individual alveoli in their walls. These bronchioles with individual alveoli in their walls are called respiratory bronchioles View Image . They characteristically exhibit a progressive reduction in height of the epithelium. The walls of respiratory bronchioles might have small knobs of smooth muscle, collagen and elastic fibers between the openings of adjacent alveoli. You can spot the knobs, but shouldn't try to distinguish the constituents, which are covered by a squamous epithelium too thin to see with the light microscope
B. Alveolar ducts The walls of alveolar ducts View Image are lined by alveoli and alveolar sacs (clusters of alveoli).
C. Alveolus The walls of these structures are covered on both sides by squamous epithelium (too thin to see) of Type I cells lining adjacent alveolar lumens. Within the walls is an extensive capillary network. You may see the space within these capillaries, or they may be filled with RBCs. The Type II pneumocytes View Image , which secrete surfactant, have large, rounded nuclei and vacuolated cytoplasm and are often difficult to identify in the light microscope (the "vacuoles" are actually granules of phospolipids that, unfortunately, are often extracted during tissue processing). In the lumen of some alveoli, you will see macrophages, called alveolar phagocytes or dust cells View Image. While components of the alveolus may be difficult to see in normal lung tissue, pathological changes that occur in the lung as the result of congestive heart failure shown here in slide 42 from your histopathology collection View Image exaggerate many of these features making them a bit easier to see:
- Poor venous return causes dilation of the alveolar capillaries.
- Type II pneumocytes with large round nuclei and clear cytoplasm are much more numerous and can be easily seen in the alveolar walls because they proliferate in an attempt to repair damaged alveoli.
- Alveolar macrophages characteristic of this condition (also known as "heart failure" cells) become laden with brownish-black hemosiderin pigment resulting from the breakdown of erythrocytes leaking from the engorged capillaries.
Slide 129_20x (lung, H&E) View Virtual Slide
Slide 130_20x (lung, H&E) View Virtual Slide
Slide 130-1_40x (lung, H&E) View Virtual Slide
Slide 130-2_40x (lung, H&E) View Virtual Slide
Slide 132_20x (lung, H&E) View Virtual Slide
Slide 132_40x (lung, H&E) View Virtual Slide
Although it is almost impossible to appreciate in these adult tissue sections, the lung is divided into lobules with a bronchiole at the center of each lobule. The blood supply is organized according to the lobule:
A. Large, thin-walled pulmonary arteries View Image run alongside the bronchi and bronchioles. These arteries are the main blood supply to the lungs. They carry large volumes of deoxygenated blood at low pressure from the right side of the heart to pulmonary capillaries in the alveoli.
B. Smaller bronchial arteries also accompany the bronchi and bronchioles. These vessels arise from the thoracic descending aorta and carry oxygenated blood at systemic pressure. They supply blood to the tissue comprising the bronchi and bronchioles and thus may be seen as part of a neurovascular bundle (artery, vein, and nerve) either in cross section View Image or longitudinal section View Image in close association with the bronchial walls. These arteries are quite a bit smaller than pulmonary arteries and for their size, have relatively thick walls.
C. Large thin-walled pulmonary veins View Image are found at the periphery of the lobules, at some distance from bronchi or bronchioles. These veins drain the intrapulmonary circulation and carry oxygenated blood (also at rather low pressure).
148 Olfactory epithelium View Virtual EM Slide
Two types of cells are shown in this EM micrograph; olfactory bipolar neurons with vesicles and cilia and supportive cells with microvilli on their apical surface. Note the absence of goblet cells in this neurosensory epithelium.
153 Trachea - Respiratory/Pseudostratified Epithelium in the Trachea View Virtual EM Slide
Compare the morphology of the goblet cells with that of the other cells of the epithelium. Note that most of them are filled with secretory product (mucus) and that they do not have cilia. The line indicates the plane of section on the next wall chart, #154.
154 Trachea - Respiratory Epithelium Respiratory Epithelium (tangential section) View Virtual EM Slide
The yellow colored area indicates the outline of one cell (see previous wall chart #153 for plane of section). Note the tops of the goblet cells protruding between the cilia. What are the differences among cilia, microvilli, stereocilia and kinocilia (which you will come across later) ? (RS3)
156 Cilia - Cross-sectioned in human trachea View Virtual EM Slide
Cross sections of cilia. The typical 9+2 arrangement of the microtubules is especially evident. The basal bodies are centrioles and have 9 triplets of microtubules with no central pair.
157 Lung - Bronchus View Virtual EM Slide
Note that the epithelium, although still pseudostratified, is not as tall as in the trachea (EM #153). Smooth muscle separates the lamina propria from the submucosa. Note the presence of a pulmonary artery and vein and that of a much smaller bronchial artery.
115 Alveoli View Virtual EM Slide
Study the organization of the alveoli. Note that individual alveoli border on each other and therefore share the wall, which is referred to as alveolar septum. Within the septum are found capillaries. Be able to recognize type I cells, type II cells and macrophages. Type II cells secrete surfactant and can be identified on the basis of their lamellar or multilamellate bodies, which cannot be seen well at this magnification. The type I cell lining the alveolus is also better identified at higher magnification (see EM #161).
161 Lung - Alveolus Alveolus (Blood-Air Barrier) View Virtual EM Slide
Study the cellular and acellular components of the blood air barrier. Also study the type II pneumocyte in the upper right corner of this micrograph. Unfortunately, the lamellar bodies are not well preserved in this preparation.
Click on a question to reveal the answer.
What is the significance of the different types of epithelium on the false and true vocal cords?
The clinical significance of nearly any epithelial tissue transition in the body is an increased propensity for cancer in these areas. The transition from the respiratory epithelium of the false vocal cord to the stratified squamous non-keratinizing epithelium of the true vocal fold is a common location for the formation of laryngeal cancer.
What are the differences among pulmonary arteries and veins and bronchial arteries?
Pulmonary arteries are a part of a low-pressure system (pulmonary blood pressure is much lower than systemic) and, therefore, have thinner walls. Pulmonary arteries are large and accompany the respiratory tree throughout the lung. Bronchial arteries are part of a high-pressure system and have a much thicker wall (in relation to lumen size) than do pulmonary arteries. Bronchial arteries are very, very small (not much bigger than an arteriole or vasa vasora) and aren’t seen below the level of the bronchus. Pulmonary veins, like pulmonary arteries, are large and are found in the parenchyma further away from the bronchi/bronchioles/etc. In summary, if a vessel is large and thin walled and traveling alone through the parenchyma, it’s probably a pulmonary vein. If it is large and thin walled and traveling along the respiratory tree, it’s probably a pulmonary artery. If it is very small, thick walled and traveling along the bronchus, it is most likely a bronchial artery.
What are the differences among cilia, microvilli, stereocilia and kinocilia (which you will come across later)?
As you learned earlier, cilia have axonemes, which are composed of microtubules. A cilium can move independently. This motion is crucial in the respiratory track to keep the lungs free of debris. Microvilli (located in the GI tract, among other places) have an actin filament core. Microvilli are much smaller than cilia and are not capable of movement but are used more to increase surface area for absorption. Stereocilia (found in the ear, male reproductive tract) are not true cilia at all. This is a misnomer. It is, in fact, a very long microvillus and, as such, contains actin filaments. Kinocilia (also found in the ear) are true cilia and contain microtubules.
1. The red line indicates the lumen of what structure?
View Image
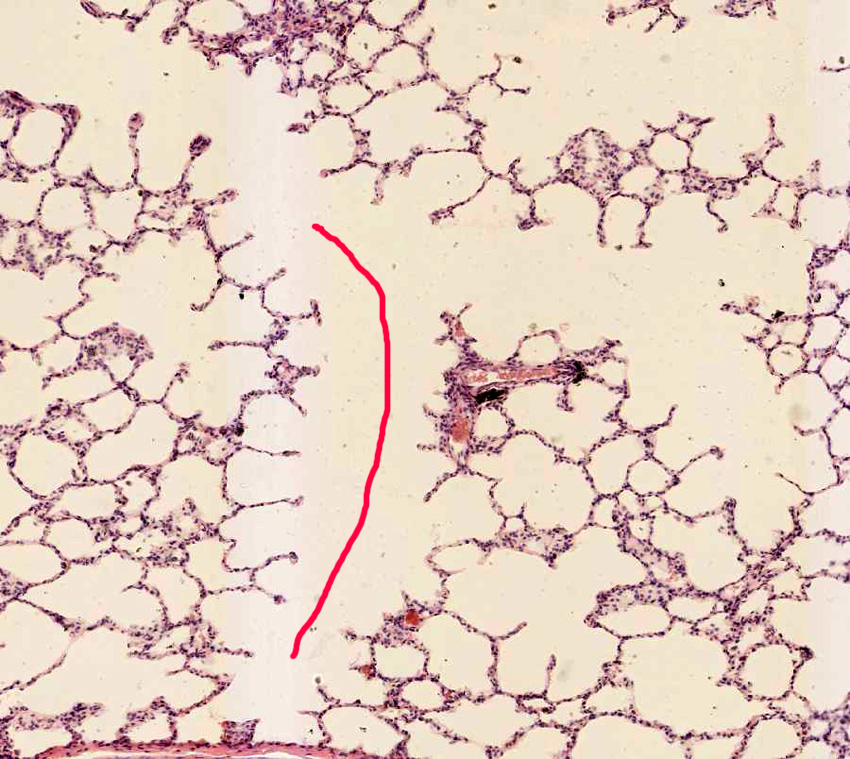
- An alveolus
- An alveolar duct.
- A respiratory bronchiole.
- A terminal bronchiole.
- A pulmonary vein.
Answer
Correct answer 2. An alveolar duct as the entire wall is lined by alveoli.
2. Identify the correct statement(s) about the cell that is marked by the black arrow.
View Image

- It is found only in the conducting portions of the respiratory tract.
- It clears foreign material from the alveolar wall.
- It produces surfactant.
- It secretes mucus.
- It is severely affected in individuals with Kartagener's syndrome.
- All of the above statements are true.
- None of the above statements is true
Answer
Correct answer 3. As the marked cell is a type II pneumocyte (note the multi-lamellar bodies in its cytoplasm), its main function is the production of surfactant.
3. Identify the segment of the respiratory tract from which this image was taken.
View Image
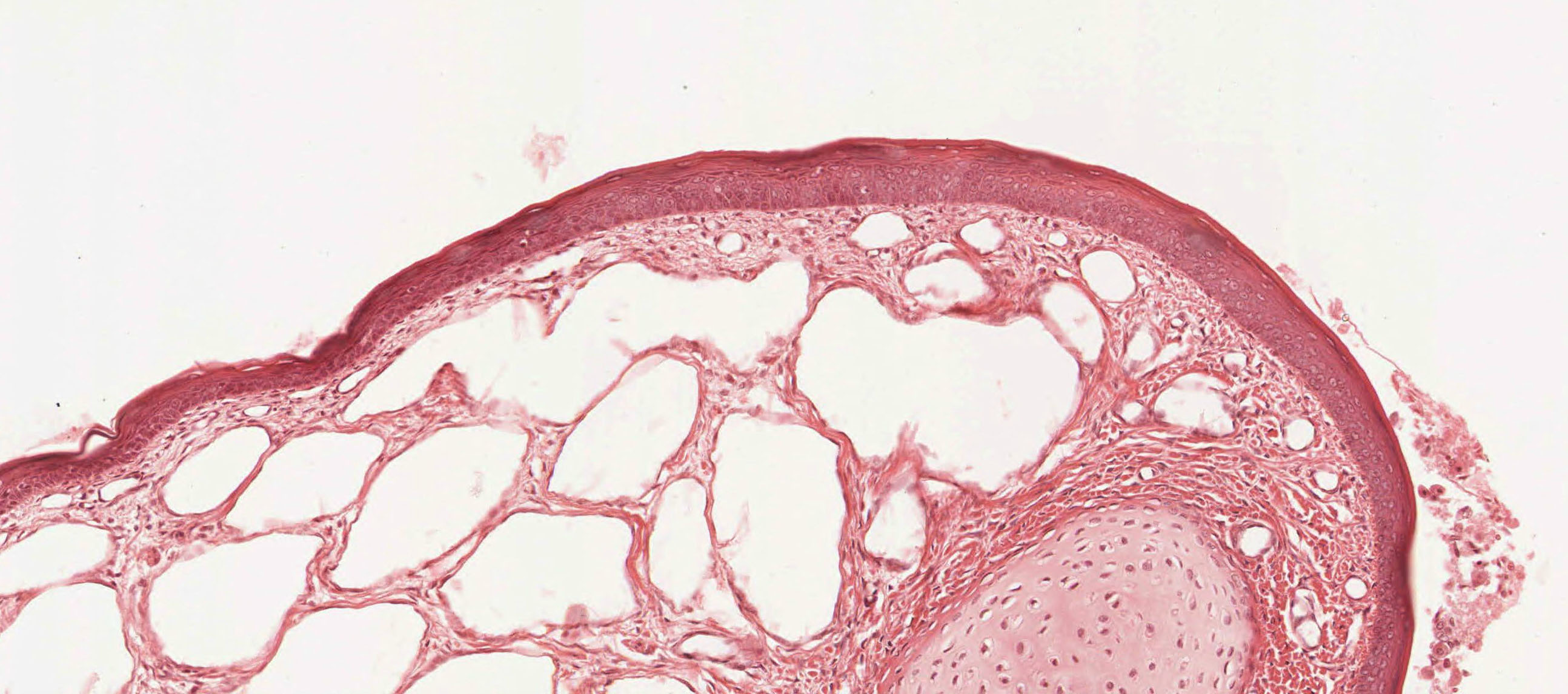
- False vocal fold.
- True vocal fold.
- Trachea
- Olfactory epithelium.
- Nasal vestibule.
Answer
Correct answer 5. This image depicts the nasal vestibule. Note the stratified squamous epithelial lining in combination with the venous sinuses.
4. Which part(s) of the respiratory tract does NOT have glands?
- Nasal cavity.
- Larynx
- Trachea
- Bronchi
- Bronchioles
Answer
Correct answer 5. Bronchioles do not have any type of gland. However, their epithelial lining contains secretory club cells.
5. Identify the part of the respiratory system depicted in this micrograph.
View Image
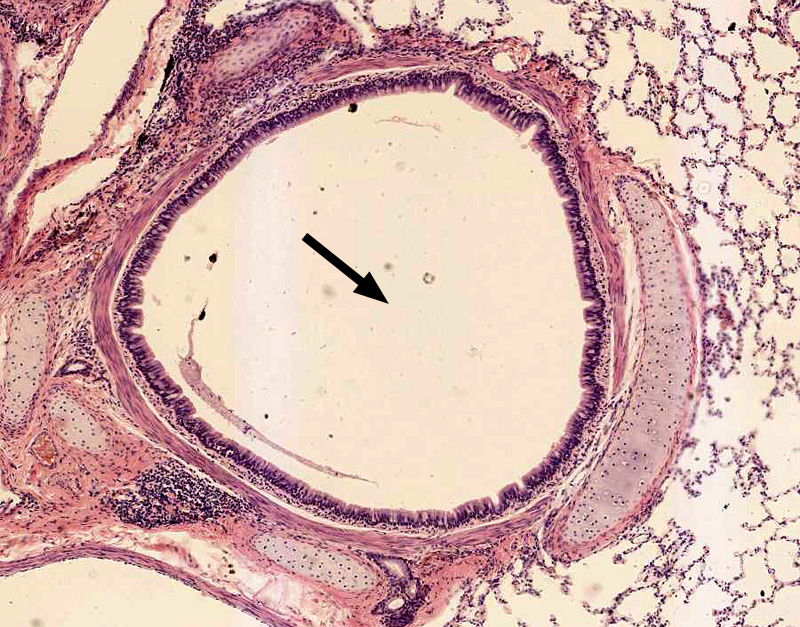
- Trachea
- Bronchus
- Bronchiole
- Bronchial artery.
- Pulmonary artery.
Answer
Correct answer 2. A bronchus as it is lined by respiratory epithelium and hyaline cartilage chips are evident in the bronchial wall.
